Placebo Effect and Generics: How Psychology Affects Your Medication Results
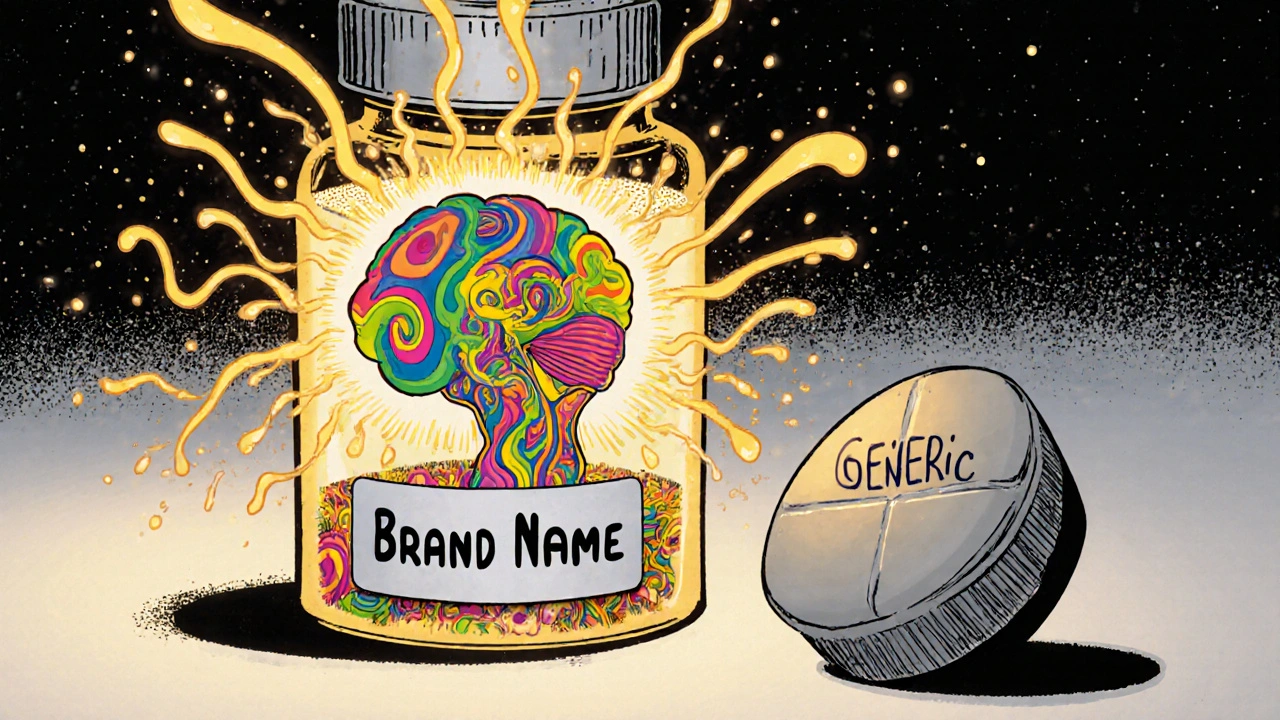
Switching from a brand-name drug to a generic might save you money-but what if your body doesn’t believe it’s the same medicine? It’s not just about chemistry. It’s about what your brain expects.
Why Your Brain Thinks Generics Don’t Work
You’ve probably heard it before: generics have the same active ingredients as brand-name drugs. They’re tested, approved, and legally required to be bioequivalent. But if you’ve switched and felt like something’s off-less energy, more anxiety, worse pain-you’re not imagining it. The problem isn’t the pill. It’s the label. A 2014 study from the University of Auckland showed this clearly. People given fake painkillers labeled as "ibuprofen" (a brand name) reported just as much relief as those who got real ibuprofen. But when the exact same placebo was labeled as a generic, pain relief dropped by nearly 40%. The pill didn’t change. The belief did. fMRI scans revealed something even more striking: when people thought they were taking a brand-name drug, their brains lit up 27% more in areas linked to pain control. That’s not magic. That’s biology. Your expectations trigger real chemical changes in your body. When you trust the name on the bottle, your brain releases natural painkillers, lowers stress hormones, and improves blood flow-all without a single active ingredient.The Cost-Per-Pill Illusion
Here’s where it gets even more powerful: price shapes perception. In a famous 2008 study, volunteers received fake painkillers. Half were told each pill cost $2.50. The other half were told they cost 10 cents. The expensive ones worked better-64% more pain relief. Even though they were identical placebos. This isn’t just about greed or marketing. It’s about a deep-seated cultural belief: expensive = better. That’s why some patients refuse generics. Not because they’re informed. Because they’re conditioned. In antidepressant trials, patients switched to generic sertraline were 22% more likely to quit treatment because they felt it “wasn’t working.” Their blood levels were identical to when they took the brand. But their brains didn’t believe it. And that’s enough to derail recovery.Generics Aren’t the Problem-Misinformation Is
Let’s clear up a myth: generics aren’t inferior. The FDA requires them to deliver the same amount of active ingredient into your bloodstream within a narrow range (80-125% of the brand). That’s not a loophole. That’s precision. If your body absorbs 92% of the same drug as the brand, it’s considered equivalent. That’s science. But here’s what most people don’t know: even the color, shape, and size of the pill matter. A 2019 FDA study found that changing a generic’s appearance increased patient dropout rates by 29%. Why? Because your brain associates the old pill with relief. Swap it out-even for a better-made version-and your system goes on alert. In one documented case, a patient stopped taking generic escitalopram after reporting “worse anxiety.” Blood tests confirmed the same drug levels as before. But the pill looked different. That was enough to trigger a nocebo response-the evil twin of the placebo effect. Your brain expects something bad to happen… and then it does.
What Works: How Doctors Can Help
The good news? This isn’t hopeless. A 2021 JAMA study tested a simple 3-minute conversation with patients switching to generics. Doctors explained three things:- Generics meet the same strict FDA standards as brand-name drugs.
- It’s normal to feel like it’s different at first-but that’s your mind adjusting, not the medicine failing.
- Give it two weeks. Your body needs time to recalibrate.
When Generics Really Don’t Work (And When They Do)
There are rare cases where generics cause issues-not because of psychology, but because of formulation. For drugs with a narrow therapeutic window-like warfarin, levothyroxine, or certain seizure meds-even tiny differences in how the body absorbs the drug can matter. That’s why some doctors prefer to stick with one brand in these cases. But here’s the twist: even in these cases, studies show that switching between FDA-approved generics doesn’t cause harm for most people. The real problem? Fear. A 2016 study found brand-name users had 18% higher adherence rates for heart meds-even when the generic was identical. That’s not because the generic was less effective. It’s because people believed it was. On the flip side, patients who were unaware they switched to generics reported the same results as those on brand-name drugs. No drop in effectiveness. No increase in side effects. Just… the same medicine. That’s the power of expectation.
What You Can Do Right Now
If you’re switching to a generic:- Don’t assume it won’t work. Your brain might be the only thing holding you back.
- Ask your pharmacist or doctor to explain the bioequivalence standards. Knowledge reduces fear.
- Give it two weeks. Your body needs time to adjust-not to the drug, but to the new idea of it.
- If you feel worse, don’t assume it’s the medicine. Ask: “Could this be my mind?” Then talk to your provider.
- Keep the same pill shape and color if possible. Don’t let a packaging change trigger a nocebo response.
- Don’t say, “It’s the same.” Say, “It’s the same medicine, but your brain might need time to trust it.”
- Use the FDA’s free patient guide. It’s clear, simple, and trusted.
- Track adherence after switching. You’ll see fewer dropouts when you address expectations upfront.
The Bigger Picture
The placebo effect isn’t a trick. It’s a feature of how human biology works. And in a healthcare system where generics make up 90% of prescriptions but only 23% of spending, ignoring psychology isn’t smart-it’s expensive. A 2021 estimate found that unnecessary brand-name prescriptions due to placebo-driven beliefs cost the U.S. healthcare system $1.4 billion a year. That’s not just money. It’s wasted trust. It’s patients who stop taking their meds because they think they’re getting second-rate care. The FDA’s 2023 pilot program now requires generic manufacturers to keep pill appearance consistent. Why? Because changing the look of a pill increases discontinuation by nearly 20%. That’s not about branding. That’s about saving lives. A new digital tool called the “Expectation Modulation Protocol” is being tested. It’s a 12-minute video that walks patients through how expectations shape medicine. In trials, it cut nocebo responses by 53%. It’s not magic. It’s education.Final Thought
Your body doesn’t care if the pill says "Lipitor" or "atorvastatin." It only cares if your brain believes it will work. And that belief? It’s something we can shape-with honest talk, clear facts, and time. The next time you’re offered a generic, don’t think about the price tag. Think about the power of your mind. And ask yourself: is my fear of the unknown stronger than my need to feel better?Do generic drugs work as well as brand-name drugs?
Yes, when approved by the FDA, generic drugs contain the same active ingredients, dosage, strength, and route of administration as their brand-name counterparts. They must meet strict bioequivalence standards-delivering between 80% and 125% of the same amount of medicine into your bloodstream. For most people, they work just as well. The difference isn’t in the chemistry-it’s in the belief.
Why do some people feel worse after switching to generics?
It’s often not the drug-it’s the expectation. If you’ve been on a brand-name pill for years, your brain links that specific shape, color, and name with relief. Switching-even to an identical generic-can trigger a nocebo effect, where your brain expects side effects or reduced effectiveness, and then your body responds accordingly. Studies show this is strongest with antidepressants, painkillers, and statins. Giving yourself two weeks to adjust, and understanding why it might feel different, often resolves the issue.
Can the color or shape of a generic pill affect how well it works?
Yes. A 2019 FDA study found that changing the appearance of a generic pill-like its color, size, or imprint-increased patient dropout rates by 29%. Your brain uses visual cues to predict how a medicine will work. If your blood pressure pill used to be white and oval, and now it’s blue and round, your brain might flag it as “different,” even if the active ingredient is identical. That’s why the FDA now encourages manufacturers to keep pill appearance consistent across generic versions.
Is it ethical for doctors to use the placebo effect to make generics work better?
It’s not about deception. It’s about honest framing. Doctors aren’t lying when they say, “This generic works the same as the brand, but your brain might need time to adjust.” That’s science. The ethical line is crossed only if a provider hides the fact that it’s a generic or pretends it’s something else. The best approach is transparency: explain the evidence, acknowledge that perception matters, and empower the patient to make an informed choice.
How can I tell if my symptoms are from the generic or something else?
Track your symptoms before and after the switch. Note timing: did the issue start within days of switching? Or was it gradual? Check your blood levels if possible-especially for drugs like thyroid meds or anticoagulants. Talk to your doctor about whether your symptoms match known side effects of the drug itself, or if they’re more aligned with anxiety about the switch. If your levels are normal and the symptoms match common nocebo patterns (fatigue, anxiety, vague discomfort), psychology is likely playing a role. Give it time. And don’t be afraid to ask: “Could this be in my head?”-because sometimes, it is.
Tina Dinh
November 30, 2025 AT 00:50This blew my mind 😱 I switched to generic sertraline last year and thought I was going crazy-suddenly super anxious, tired, blah. Turns out my brain was just mad the pill looked different! Gave it two weeks, told myself ‘it’s the same stuff’… and boom. Back to normal. Why didn’t anyone tell me this before?? 🙏
Andrew Keh
November 30, 2025 AT 14:32It is important to recognize that psychological factors can significantly influence the perceived effectiveness of medication. The evidence presented here is both compelling and well-documented. A patient’s belief system is a legitimate part of the therapeutic process and should not be dismissed as mere superstition.
tushar makwana
December 2, 2025 AT 12:11in india we use generics all the time and no one cares about the color or brand... but i saw my aunt cry when her blood pressure pill changed shape. she said 'it doesn't feel right'... i never thought about it like that. maybe it's not about the medicine, it's about the routine. the shape, the bottle, the habit. that's what makes people feel safe.
Richard Thomas
December 3, 2025 AT 09:47While the anecdotal evidence presented is intriguing, it is imperative to acknowledge the methodological limitations of small-scale behavioral studies in the context of pharmacological outcomes. The placebo effect, while empirically validated in controlled environments, cannot be extrapolated to population-level adherence patterns without controlling for confounding variables such as socioeconomic status, health literacy, and physician-patient communication dynamics.
Matthew Higgins
December 3, 2025 AT 21:19bro. i took generic Adderall for a month. felt like a zombie. thought my brain was broken. then i found out the pill was blue instead of orange. i asked my doc to switch back to the orange one (same generic, different maker) and suddenly i was back to my 120% self. it’s wild. your brain is a glitchy AI that needs the right icon.
Mary Kate Powers
December 4, 2025 AT 14:42For anyone reading this and feeling weird after switching: you’re not crazy. Your brain isn’t broken. It’s just used to a certain rhythm. Give yourself grace. Talk to your pharmacist-they can often keep you on the same look and feel even if it’s generic. And two weeks? That’s all it takes for your mind to catch up. You’ve got this 💪
Sara Shumaker
December 6, 2025 AT 12:27This isn’t just about pills-it’s about how we assign meaning to objects. The color, the shape, the brand name… they’re all symbols. We’ve built entire emotional architectures around them. When you change the symbol, even if the substance is identical, you’re asking the nervous system to rewire its expectations. That’s not irrational. That’s human. The real question is: why do we let corporations control these symbols for profit instead of designing them for healing?
Scott Collard
December 7, 2025 AT 16:12So what? You’re telling me we should pay more for brand names because people are weak-minded? That’s not medicine. That’s enabling. If your brain can’t handle a blue pill, maybe you shouldn’t be on medication at all.
Brandy Johnson
December 9, 2025 AT 05:25Let me be clear: the FDA’s approval process for generics is a joke. These companies cut corners. The fact that people ‘feel worse’ is not psychology-it’s chemistry. America is falling apart because we trust marketing over science. Stop romanticizing placebo effects. This isn’t New Age nonsense-it’s corporate fraud disguised as ‘patient care.’