When to Call Poison Control vs. Emergency Services for Overdose
When someone overdoses, every second counts. But calling the wrong service can cost time, resources, and even lives. You might think overdose always means 911 - but that’s not true. In fact, calling Poison Control first can save lives, prevent unnecessary hospital trips, and get the right help faster. The key isn’t guessing - it’s knowing the signs.
Call 911 Immediately If There Are Life-Threatening Symptoms
If the person is unresponsive, not breathing, having seizures, or their heart is racing or crashing, don’t hesitate. Call 911 right away. These are not symptoms you can wait out. The CDC reports that 28.3% of fatal poisoning cases involve respiratory arrest or severe breathing trouble. If someone isn’t waking up when you shake them or pinch their shoulder, they’re in cardiac or respiratory arrest territory. That’s a code blue situation. Other clear red flags:- Seizures lasting more than 5 minutes
- Systolic blood pressure below 90 mmHg (dizzy, cold skin, fainting)
- Blue lips or fingertips (sign of low oxygen)
- Heart rate over 140 or under 50 beats per minute
These aren’t "maybe" situations. They’re emergencies. Even if you’re unsure, call 911. Better to be wrong than to wait too long.
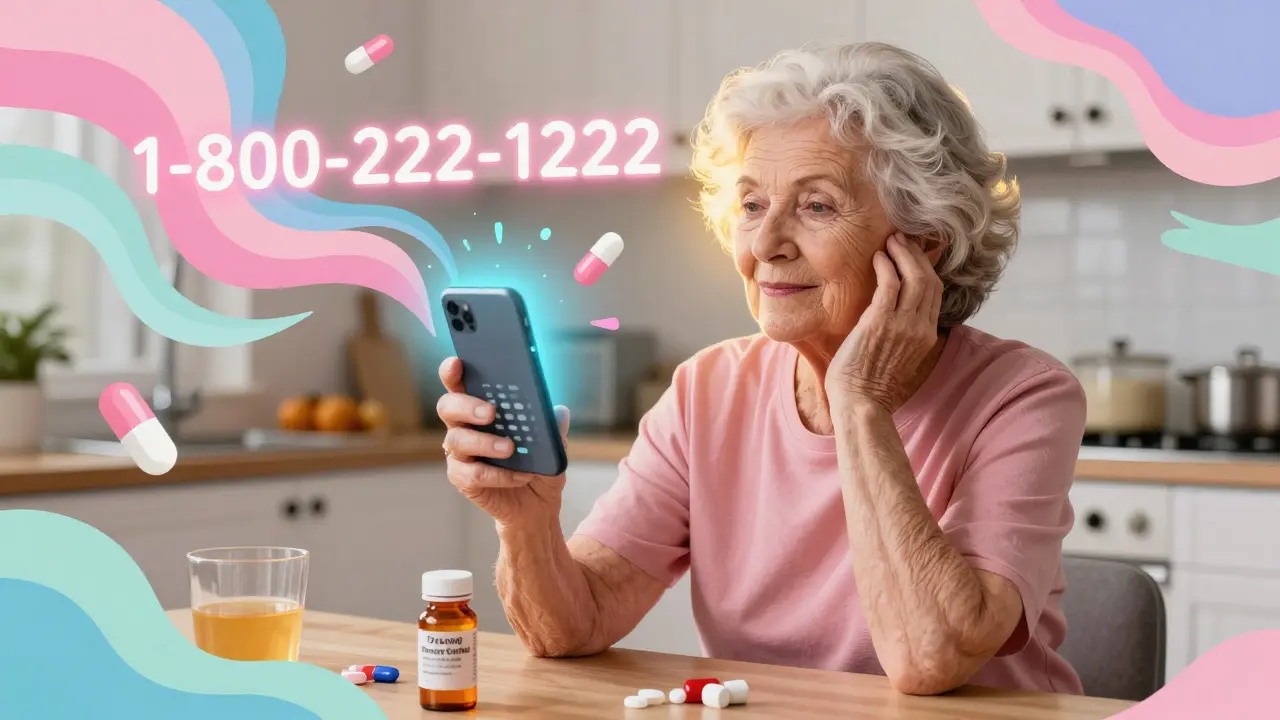
Call Poison Control First If the Person Is Stable
Poison Control isn’t just for kids who ate laundry detergent. It’s a 24/7 lifeline for adults, too. If the person is awake, breathing normally, and acting like themselves - even if they took too much medicine - call 1-800-222-1222 first. The national Poison Help hotline connects you to a toxicology expert in under a minute. In 2022, they handled over 2 million calls. You should call Poison Control if:- The person took one extra pill or a double dose of a prescription drug
- They’re alert and talking, with no changes in breathing or consciousness
- The exposure happened less than 2 hours ago
- You know exactly what was taken and how much
For example, if your 72-year-old parent accidentally took two 10mg pills of a blood pressure med instead of one, and they feel fine - call Poison Control. They’ll tell you whether to monitor at home or go to the ER. This avoids a trip that could cost $1,500+ and tie up an ambulance needed for someone in real danger.
What Information to Have Ready Before You Call
Whether you’re calling 911 or Poison Control, the more accurate your info, the better the advice. Don’t guess. Look at the container. Write it down. For Poison Control, you need:- Exact product name - "Ibuprofen" isn’t enough. Is it Advil? Motrin? Extended-release? The formulation changes everything.
- Amount ingested - "A handful" won’t cut it. Use the bottle: "2 tablets of 200mg each"
- Time of exposure - "About 45 minutes ago" is fine. Don’t say "a while ago."
- Person’s weight - Even an estimate helps. 150 lbs? 120 lbs? This affects toxicity calculations.
- Current symptoms - "They’re a little dizzy" or "No symptoms yet"
For 911, give the same info - but add location and whether you’ve given any first aid. Did you give naloxone? Did they vomit? Did you start CPR? That’s critical.

Special Cases: Kids, Seniors, and Opioids
Not all overdoses are the same. Age and substance matter.Children Under 6
About 45% of all Poison Control cases involve kids under 6. Most are accidental - a pill dropped, a bottle left open. If your child swallowed one pill and is acting normal, call Poison Control. But if they’re drowsy, vomiting, or having trouble breathing - call 911. Some medications are deadly even in tiny amounts. Clonidine (used for high blood pressure) can cause coma in kids at doses as low as 0.01 mg per kg. Sulfonylureas (diabetes meds) can crash blood sugar dangerously fast. Poison Control knows which ones to worry about.Adults Over 75
Seniors are 37% more likely to die from the same overdose as a healthy adult. Why? They’re often on 5 or more medications. A simple interaction between blood pressure pills, heart meds, and painkillers can cause sudden collapse. If an older adult takes too much of anything - even if they seem fine - get them to the ER. Don’t wait. A 2022 JAMA study found 83% of adults over 75 take five or more daily meds. That’s a recipe for hidden dangers.Opioid Overdoses
This one’s tricky. If you suspect an opioid overdose - fentanyl, heroin, oxycodone - and the person is unresponsive, give naloxone (Narcan) if you have it. Then call 911 immediately. Even if they wake up after naloxone, they still need emergency care. Fentanyl and its analogs can come back. The effects of naloxone wear off in 30-90 minutes. The opioid might still be in their system. That’s why 61% of people who initially respond to naloxone need another dose or hospital care. Don’t call Poison Control first for suspected opioid overdoses. Go straight to 911.Why Poison Control Isn’t Always the Answer
Some people try to use Poison Control as a way to avoid the ER - and that’s dangerous. A Medscape survey of emergency doctors found that 68% of them see patients who came in after being told by Poison Control to "wait and watch" - but the patient had a high-risk drug like a calcium channel blocker or beta-blocker. These drugs can cause sudden heart failure hours later. Poison Control is great for low-risk, single-substance cases. But if someone took multiple drugs, intentionally overdosed, or used street drugs - call 911. There’s no time for "maybe."Technology Can Help - But Don’t Rely on It
The webPOISONCONTROL website and mobile app let you input details and get instant advice. In 2022, nearly 30% of calls were handled online. It’s fast. It’s accurate - 97% match rate with toxicologists. But here’s the catch: it can’t handle symptoms. If the person is vomiting, confused, or having trouble breathing - you can’t use the app. It’s designed for prevention, not crisis. Also, the app doesn’t call 911 for you. It gives advice. If it says "go to the ER," you still have to call 911 or drive them. Don’t assume the app will do it for you.
What Happens When You Call?
When you call Poison Control, you’ll speak with a nurse, pharmacist, or medical toxicologist trained in poison management. They’ll ask you the questions above. Then they’ll give you step-by-step instructions:- Watch for symptoms
- Give water or milk (if safe)
- Do NOT induce vomiting unless told to
- Bring the container to the hospital if needed
They’ll also follow up. In many cases, they’ll call you back in an hour to check in. That’s how they prevent complications.
When you call 911, dispatchers send an ambulance. Paramedics are trained to handle overdoses. They carry naloxone, oxygen, IV fluids, and monitors. They’ll start treatment on the way and communicate with the ER before arrival.
Final Rule: When in Doubt, Call 911
The safest rule? If you’re unsure, call 911. It’s better to have an ambulance show up and it turn out to be nothing than to wait and lose precious minutes. Poison Control is a tool - not a replacement for emergency care. Use it for stable, known exposures. Use 911 for anything that feels wrong.And remember: this service is free. Confidential. Available 24/7. You don’t need insurance. You won’t get billed. And you’re not "bothering" anyone. That number - 1-800-222-1222 - is there because lives depend on it.
Can I call Poison Control for a suspected drug overdose?
Yes - but only if the person is awake, breathing normally, and you know exactly what they took. If they’re unresponsive, having seizures, or you suspect opioids like fentanyl, call 911 instead. Poison Control is best for accidental, single-substance overdoses in stable people.
Is it safe to wait and see if symptoms develop?
For some exposures, yes. Most pharmaceutical overdoses (like acetaminophen or ibuprofen) take 4-6 hours to cause serious harm. If the person is alert and has no symptoms after 1 hour, they’re likely low-risk. But if they took multiple drugs, have heart or liver problems, or are over 75 - don’t wait. Call 911 immediately.
Do I need to go to the ER after calling Poison Control?
Sometimes. Poison Control may tell you to monitor at home - or they may say to go to the ER. If they recommend going, don’t delay. Even if they say "no," watch the person closely for the next 6 hours. Symptoms can appear suddenly, especially with extended-release pills or unknown substances.
What if I don’t know what was taken?
Call 911. If you’re unsure what the person took - whether it’s pills, chemicals, or unknown substances - emergency services are the only safe option. Poison Control needs specifics to help. Without them, they can’t give accurate advice.
Can I use the Poison Control app instead of calling?
The app is useful for low-risk situations where the person has no symptoms and you have full details. But if there’s any doubt - if the person is acting strange, drowsy, or has taken unknown substances - call 1-800-222-1222 or 911. The app can’t assess symptoms or replace human judgment.
Jonathan Noe
February 12, 2026 AT 08:51Let me tell you something most people don't get - Poison Control isn't a backup plan, it's the first line of defense. I work in ER nursing and I've seen too many ambulances sent out for someone who took two extra Tylenol and was perfectly fine. The system gets clogged because people panic and call 911 like it's a fire alarm. Poison Control has access to real-time toxicology databases that 99% of ER docs don't even have on their phones. Use the damn number.
Jim Johnson
February 13, 2026 AT 22:50yo this is straight fire 🙌 i had my grandma take 2x her blood pressure med last month and i called Poison Control first - they told me to give her water, watch her for 90 mins, and if she didn't get dizzy, she was good. no hospital, no bill, no stress. they even called back an hour later. that's next level care. y'all need to save 1-800-222-1222 in your phone right now. not later. now.
Vamsi Krishna
February 15, 2026 AT 04:12you know what's funny? Americans think they're so smart with their apps and hotlines but in India we just know - if someone stops breathing, you slap them and run. no time for protocols. Poison Control? That's a luxury for people who have time to wait for a nurse to answer. Here, we have 5 people in one house, 3 of them on meds, and we just eyeball it. If they look dead, we call an auto rickshaw. If they look sleepy, we give them chai. Simple. No forms. No wait. No bureaucracy. You're overcomplicating survival.
Brad Ralph
February 16, 2026 AT 18:21so we’re saying if you’re not dead yet, call a pharmacist? 🤔
and if you’re kinda dead? call 911.
and if you’re kinda kinda dead? call 911 anyway because you’re too scared to be wrong.
and if you’re not sure? call 911 because the algorithm of fear is more reliable than the algorithm of knowledge.
we’ve turned medicine into a choose-your-own-adventure book written by lawyers.
Steve DESTIVELLE
February 18, 2026 AT 05:25the truth is no one really cares about protocols until it happens to them then suddenly everyone becomes an expert on toxicology and emergency response but let me ask you this what is life if not a series of unpredictable chemical reactions and what is death if not the final imbalance of ions in the body and if we are all just collections of molecules then why do we need to label every reaction as emergency or non emergency why not just let nature take its course and stop pretending we can control the uncontrollable
Stephon Devereux
February 19, 2026 AT 10:56if you're reading this and you haven't saved Poison Control in your phone yet - stop. right now. open your contacts. type in 1-800-222-1222. name it 'POISON HELP'. do it. I'm not joking. This isn't about being prepared - it's about being responsible. You think you'll never need it? Your kid might grab a pill. Your mom might mix meds. Your partner might take an extra sleep aid. This number costs nothing. It saves time. It saves money. It saves lives. Do it. Now.
steve sunio
February 21, 2026 AT 07:39poison control is just a glorified chatbot with a phd. they tell you to 'monitor' and then the next day the person is in a coma because 'monitoring' is just a fancy word for waiting around hoping nothing bad happens. 911 is the only real option. if you're not calling 911 you're just gambling with someone's life and i dont trust any system that says 'wait and see' when someone's brain might be turning to mush
Neha Motiwala
February 22, 2026 AT 01:04I knew this was coming. I knew it. The system is rigged. Poison Control is funded by pharmaceutical companies. They want you to call them so they can avoid hospital liability. Did you know that in 2021, 4 out of the 7 top Poison Control advisors had stock in Bayer? And they told people to 'wait and watch' after a fentanyl exposure? That's not advice - that's corporate sabotage. I have a cousin who died because they listened to Poison Control. She was fine for 4 hours. Then she stopped breathing. No one was ready. No one was watching. The system failed us.
Jonathan Noe
February 23, 2026 AT 00:02^ I get why you’re skeptical, but you’re conflating funding with competence. Poison Control is federally funded - the CDC monitors them. Their advice is peer-reviewed. If you think they’re pushing pharma agendas, then explain why they told a guy to go to the ER after he took a single 10mg dose of diltiazem. That’s a cardiac bomb. They flagged it immediately. They’re not selling you snake oil - they’re saving you from it.