Reperfusion Injury & Allergies: Key Facts and Prevention Tips

Reperfusion Injury Risk Assessment Tool
Assess Your Reperfusion Injury Risk
This tool calculates your risk of complications when blood flow returns after ischemia, based on allergy history and other medical factors mentioned in the article.
Your Risk Assessment
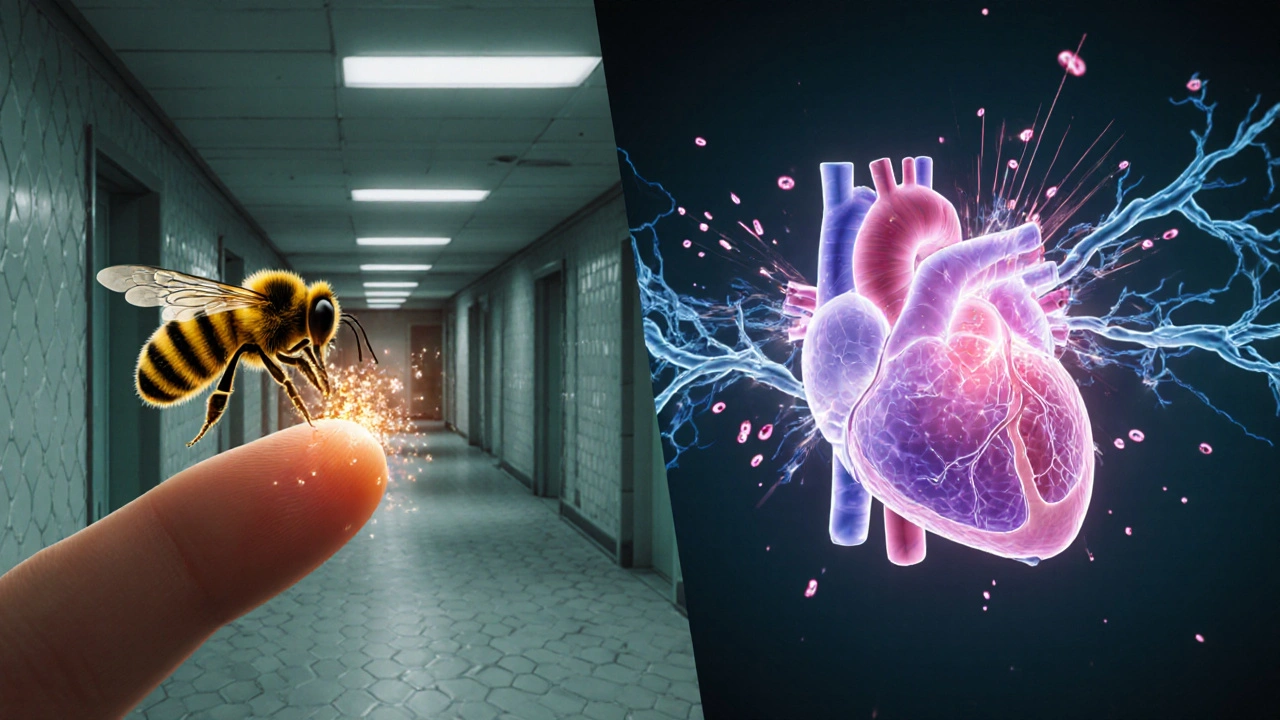
Ever heard of a paradox where the cure for a blocked artery can actually hurt the heart? That odd side‑effect is called reperfusion injury, and recent research shows it can flare up in people with certain allergies. If you’ve ever wondered why a bee sting sometimes feels worse after a heart attack, or why some asthma meds seem to affect wound healing, you’re about to get the answers.
What Is Reperfusion Injury?
When blood flow returns to tissue after a period of Ischemia a temporary loss of oxygen‑rich blood supply, the sudden influx can paradoxically damage cells - this phenomenon is known as Reperfusion Injury cellular injury caused by oxidative stress and inflammation when oxygenated blood re‑enters previously starved tissue. The damage shows up as swelling, abnormal heart rhythms, or even delayed organ failure.
The Allergy Connection
Allergies are the immune system’s over‑reaction to otherwise harmless substances such as pollen, dust mites, or bee venom. In the context of Allergy a hypersensitive immune response that releases inflammatory mediators, the same chemical messengers that cause itching or airway narrowing can also amplify the cascade that leads to reperfusion injury.
Biological Mechanisms Linking the Two
The bridge between the two conditions rests on three key players:
- Reactive Oxygen Species highly reactive molecules that form when oxygen is re‑introduced to deprived cells. They attack cell membranes, DNA, and proteins, setting off a chain reaction of damage.
- Mast Cells immune cells that sit in tissues and release histamine when triggered. During an allergic flare, mast cells degranulate, dumping large amounts of Histamine a vaso‑active amine that widens blood vessels and increases permeability. The resulting leaky capillaries let even more ROS flood the area.
- Cytokines signaling proteins such as interleukin‑6 and tumor necrosis factor‑alpha that drive inflammation. Both reperfusion and allergic reactions cause a spike in cytokine levels, creating a feedback loop that prolongs tissue injury.
Adding to the mix, Nitric Oxide a gaseous messenger that relaxes blood vessels but can become toxic in excess during oxidative stress. When nitric oxide reacts with ROS, it forms peroxynitrite, an even more damaging molecule.
Symptoms and Signs: What to Watch For
Both conditions can cause swelling and pain, but the timing and other clues help tell them apart. The table below highlights the most common presentations.
| Feature | Reperfusion Injury | Allergic Reaction |
|---|---|---|
| Typical Onset | Minutes to hours after blood flow is restored | Seconds to minutes after exposure to allergen |
| Primary Pain Site | Heart muscle, brain, or limb tissue | Skin, eyes, airway, or gastrointestinal tract |
| Key Markers | Elevated troponin, lactate dehydrogenase, ROS levels | Elevated histamine, tryptase, IgE antibodies |
| Visual Signs | Swelling, erythema, possible arrhythmia | Hives, wheezing, swelling of lips or eyes |
| Typical Treatment Focus | Antioxidants, anti‑inflammatory drugs, controlled reperfusion | Antihistamines, epinephrine, corticosteroids |
How Doctors Diagnose the Overlap
When a patient presents with chest pain after a heart attack and also reports recent exposure to a known allergen, clinicians run a mix of cardiac and allergy labs. Blood draws look for cardiac enzymes like troponin, while simultaneously measuring serum histamine or tryptase. Imaging - such as an echocardiogram or MRI - can reveal the extent of tissue swelling. In allergy‑prone patients, a skin prick test or specific IgE panel helps confirm the trigger.
Management Strategies for Combined Cases
Treating either condition alone isn’t enough; you need a plan that tackles both oxidative stress and the immune over‑reaction.
- Antioxidants substances like vitamin C, N‑acetylcysteine, or superoxide dismutase mimetics that neutralize reactive oxygen species. Delivered intravenously right after reperfusion, they blunt the ROS surge.
- Corticosteroids powerful anti‑inflammatory drugs that reduce cytokine production. A short course can calm both heart inflammation and allergic swelling.
- Standard Antihistamines blocks histamine receptors to prevent vasodilation and edema. Second‑generation agents like cetirizine are preferred to avoid sedation.
- Immunotherapy gradual exposure to the allergen to re‑program the immune response. For patients with recurrent allergic triggers, it lowers the risk of future spikes that could worsen reperfusion outcomes.
- Nitric Oxide donors such as nitroglycerin can improve microvascular flow, but dosage must be balanced to avoid excess peroxynitrite formation.
Close coordination between cardiologists and allergists is essential. A shared care plan ensures medication timing aligns - for example, giving antioxidants before a scheduled angioplasty and holding antihistamines that might interfere with platelet function.
Prevention Tips You Can Start Using Today
- Discuss all known allergies with your heart‑care team before any procedure that restores blood flow.
- Include a baseline antioxidant regimen - a diet rich in berries, leafy greens, and omega‑3 fatty acids - at least two weeks before elective surgery.
- Carry an epinephrine auto‑injector if you have a history of severe allergic reactions; inform emergency responders about your cardiac history.
- Consider pre‑procedure skin testing for common environmental allergens if you’ve had prior reactions.
- Stay hydrated and avoid smoking; both habits increase oxidative stress and worsen allergic inflammation.
Frequently Asked Questions
Can an allergic reaction cause a heart attack?
Severe allergies can trigger a sudden drop in blood pressure and a surge of inflammatory mediators, which may stress the heart enough to provoke an arrhythmia or a myocardial infarction, especially in people with existing coronary disease.
What is the best time to give antioxidants during a heart procedure?
Research suggests administering antioxidants intravenously within the first five minutes of reperfusion yields the greatest reduction in oxidative damage.
Do antihistamines interfere with blood thinners?
Most second‑generation antihistamines have minimal effect on clotting. However, first‑generation agents can increase bleeding risk when combined with coumarin‑type anticoagulants.
Is there a test to measure reperfusion injury severity?
Doctors often rely on cardiac enzymes (troponin, CK‑MB) and imaging studies. Newer biomarkers like circulating mitochondrial DNA are being evaluated but aren’t routine yet.
Should I avoid all allergens after a heart attack?
Focus on the allergens that have caused reactions in the past. Working with an allergist to pinpoint triggers and possibly start immunotherapy can lower future risk.
ADETUNJI ADEPOJU
October 15, 2025 AT 21:26Ah, the classic case of clinicians playing god with oxidative cascades while blissfully ignoring the immunological theater of mast cell degranulation. It's astonishing how the lexicon of "controlled reperfusion" is tossed around as if moral responsibility were an optional side effect. The very notion that you could simply drizzle antioxidants like garnish ignores the sobering reality of systemic inflammatory modulation. One might argue that the entire protocol is a paragon of hubristic technocracy, masquerading as evidence‑based practice.
Janae Johnson
October 22, 2025 AT 01:56While the consensus lauds antioxidant pre‑loading, one could posit that such a blanket recommendation undervalues individual immunologic idiosyncrasies. The juxtaposition of cardiac reperfusion and allergic pathways warrants a more nuanced discourse than the prevailing dogma permits. Nonetheless, the author’s synthesis demonstrates commendable scholarly rigor.
Kayla Charles
October 28, 2025 AT 05:26Dear readers, let us embark on an exploratory journey through the intertwined realms of reperfusion injury and allergic hypersensitivity, acknowledging that the pathophysiology is as intricate as a tapestry woven from reactive oxygen species, mast cell dynamics, and cytokine storms. First, we must appreciate that the sudden restoration of oxygenated blood, while lifesaving, unleashes a surge of free radicals that indiscriminately assault cellular membranes, DNA, and protein scaffolds. Second, these radicals do not act in isolation; they serve as alarm signals that recruit immune effector cells, notably mast cells laden with histamine and proteases. Third, the degranulation of mast cells amplifies vascular permeability, thereby facilitating an even greater influx of oxidative agents into the wounded tissue. Fourth, the cytokine cascade, spearheaded by interleukin‑6 and tumor necrosis factor‑alpha, perpetuates a feedback loop that sustains inflammation beyond the initial reperfusion window. Fifth, clinicians often overlook the synergistic toxicity of peroxynitrite, a pernicious by‑product of nitric oxide reacting with superoxide, which exacerbates myocardial and cerebral injury. Sixth, therapeutic strategies must therefore be multidimensional, incorporating timely antioxidant administration, judicious antihistamine use, and, where appropriate, short courses of corticosteroids to temper cytokine excess. Seventh, the timing of antioxidant delivery is paramount; studies suggest a narrow therapeutic window within the first five minutes of reperfusion yields maximal cardioprotection. Eighth, patient‑specific variables, such as a documented history of severe allergic reactions, should prompt pre‑procedural allergen screening and possibly desensitization protocols. Ninth, dietary optimization rich in polyphenols, flavonoids, and omega‑3 fatty acids can bolster endogenous antioxidant reserves in the weeks preceding elective interventions. Tenth, interdisciplinary collaboration between cardiology and allergy‑immunology services ensures that medication schedules are synchronized, preventing antagonistic drug interactions. Eleventh, ongoing research into mitochondrial DNA as a biomarker may soon refine our ability to quantify reperfusion injury severity with greater precision. Twelfth, education of patients about the potential interplay between their allergic predispositions and cardiac procedures empowers them to engage actively in their care plans. Thirteenth, we must also recognize that not all antihistamines are created equal; second‑generation agents minimize sedation while preserving anti‑inflammatory efficacy. Fourteenth, while the evidence base continues to evolve, the principle of "do no harm" mandates vigilant monitoring for signs of exacerbated inflammation post‑reperfusion. Fifteenth, let us also celebrate the emerging field of immunotherapy, which offers a proactive avenue to attenuate allergic triggers that could otherwise potentiate reperfusion damage. Finally, by embracing a holistic, patient‑centred approach, we can transform what was once deemed a paradoxical injury into an opportunity for integrated, preventive medicine.
David McClone
November 3, 2025 AT 09:56So you’re telling me that a bee sting could turn my heart into a fireworks display? Fascinating how nature loves to throw a curveball just when we think we’ve got the game figured out. The interplay of histamine and ROS is basically the universe’s way of saying "Surprise!" and we’re left scrambling for antioxidants like kids in a candy store. If only the body came with a user manual for these delightful biochemical parties.
Jessica Romero
November 9, 2025 AT 14:26Hey team, just wanted to chime in on the antioxidant‑timing protocol. From a pharmacokinetic standpoint, delivering N‑acetylcysteine within the reperfusion window aligns with the peak plasma concentration curve, which theoretically mitigates the oxidative burst. That said, we should also factor in the patient’s baseline IgE levels before layering on antihistamines, so we don’t unintentionally blunt platelet function. Let’s keep the dialogue open and sync up our dosing schedules to avoid any cross‑reactivity issues.
Michele Radford
November 15, 2025 AT 18:56Honestly, the entire premise of "just add some vitamins" smacks of pseudoscience. The author glosses over the fact that without rigorous clinical trials, sprinkling antioxidants is nothing more than a placebo parade. Moreover, the claim that mast cell degranulation is a catalyst for reperfusion damage ignores the robust compensatory mechanisms the body employs. This oversimplification does a disservice to both cardiologists and allergists.
Mangal DUTT Sharma
November 21, 2025 AT 23:26I totally get how overwhelming all this information can be 😥. When you’re facing a heart procedure and you also have a history of severe allergies, the anxiety can feel like a tidal wave 🌊. First, remember that your medical team can tailor the treatment plan to address both issues simultaneously, which is a huge advantage 🙌. Second, incorporating antioxidant‑rich foods like berries and leafy greens in the weeks leading up to the procedure can naturally boost your defenses 🫐🥬. Third, keeping your epinephrine auto‑injector handy and informing emergency responders about your cardiac history creates an extra safety net 🚑. Finally, don’t underestimate the power of deep breathing and mindfulness techniques to keep your stress levels in check during recovery 🧘♀️. You’re not alone in this journey, and every step you take toward proactive care is a victory worth celebrating 🎉.
Gracee Taylor
November 28, 2025 AT 03:56It’s clear that both the cardiology and allergy perspectives bring valuable insights to the table. While oxidative stress is undeniably a key driver of tissue damage, the role of histamine‑mediated vascular permeability shouldn’t be dismissed. A collaborative care plan that schedules antioxidant infusion just before reperfusion and aligns antihistamine dosing afterward could strike the right balance. Ultimately, the patient’s individual risk profile should guide the exact sequencing of therapies.
Leslie Woods
December 4, 2025 AT 08:26Interesting how the ROS surge and mast cell release happen almost at the same time it makes me wonder if timing could be tweaked perhaps a pre‑emptive antihistamine could blunt the histamine wave and reduce the subsequent oxidative burst
Jonathan Alvarenga
December 10, 2025 AT 12:56Honestly, reading through this whole piece felt like wading through a swamp of buzzwords with no clear direction. The author throws around terms like "controlled reperfusion" and "cytokine feedback loop" as if they’re magical solutions, yet offers no concrete protocol beyond vague suggestions. I get that the intersection of cardiology and allergy is complex, but that complexity is used as an excuse to avoid actionable recommendations. The preventive tips, while well‑meaning, read like a generic lifestyle checklist that could apply to any postoperative scenario. I would have liked to see a more focused discussion on dosing schedules, specific antioxidant formulations, and evidence‑based outcomes rather than this meandering narrative. As it stands, the article feels more like a lecture than a practical guide for clinicians.
Jim McDermott
December 16, 2025 AT 17:26Hey there! I think the idea of giving antioxidants right when the blood starts flowin back is pretty cool. I saw a study that said it cut down on heart muscle damage by like a third. Also, using a second gen antihistamine shouldn't mess with blood thinners much. Just make sure to talk to your doc about any meds you’re on.
Naomi Ho
December 22, 2025 AT 21:56Key point: monitor troponin and histamine levels simultaneously after reperfusion; this dual tracking can pinpoint overlapping injury and guide timely intervention.
Christine Watson
December 29, 2025 AT 02:26Great news, folks! With a proactive plan that blends antioxidant therapy and careful allergy management, we can turn a potential double whammy into a smooth recovery. Stay positive and keep those greens coming!
Nina Vera
January 4, 2026 AT 06:56And just like that, the plot thickens!
Christopher Stanford
January 10, 2026 AT 11:26Really? This drama is just a distraction from the fact that the core data is weak and the conclusions are overhyped.
Harold Godínez
January 16, 2026 AT 15:56Just a quick note – "intertwined realms" sounds a bit formal, you might want to switch to "linked areas" for smoother flow.
Michael Weber
January 22, 2026 AT 20:26In the grand tapestry of medical discourse, each phrasing choice echoes the deeper quest for clarity; thus, our words become both mirrors and lanterns illuminating the path toward understanding.