Psoriasis and Psoriatic Arthritis: Understanding the Autoimmune Link Between Skin and Joints
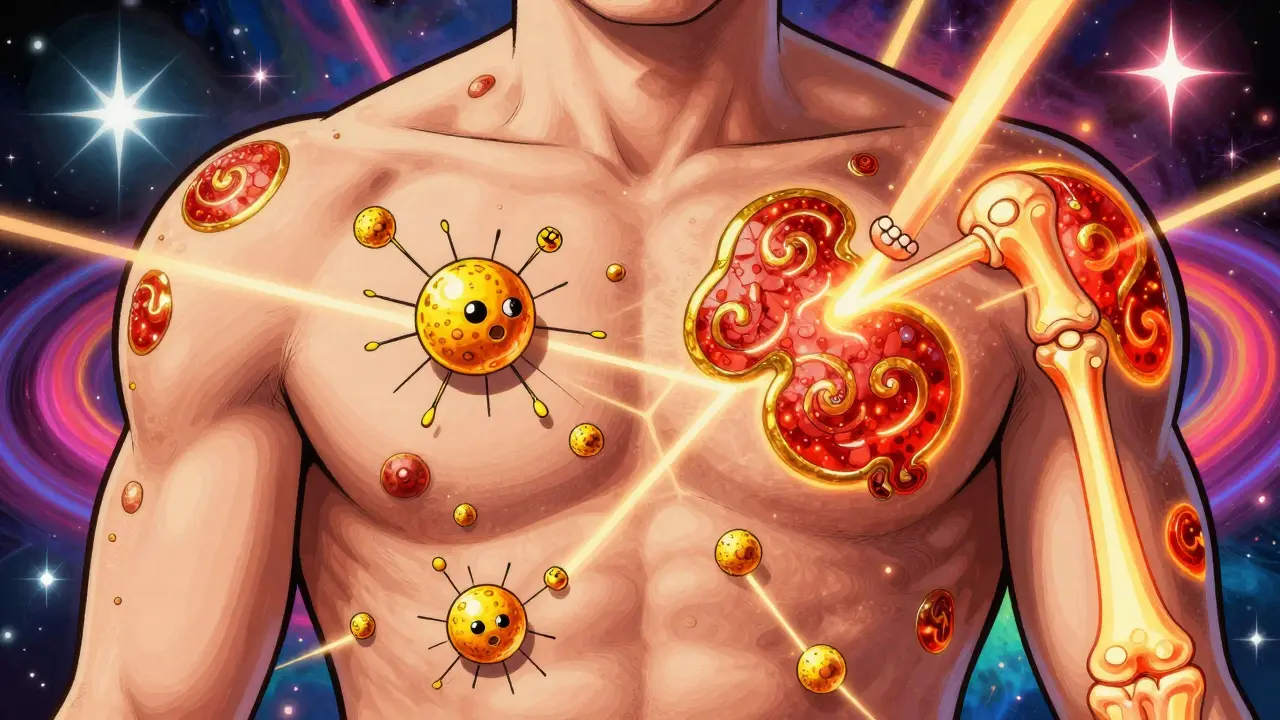
When your skin breaks out in red, scaly patches and your fingers swell like sausages, it’s not just bad luck-it’s your immune system turning on you. Psoriasis and psoriatic arthritis (PsA) are two sides of the same autoimmune coin. One attacks your skin. The other attacks your joints. But they don’t happen by accident. They’re linked. And if you have one, you’re at risk for the other.
What Exactly Is Psoriasis?
Psoriasis isn’t just dry skin. It’s an autoimmune condition where your body sends the wrong signals. Immune cells mistake healthy skin cells for invaders and rush to attack them. This speeds up skin cell growth from weeks to days. Dead cells pile up before they can shed, forming thick, silvery plaques. These show up on elbows, knees, scalp, and lower back. About 80-90% of people with psoriatic arthritis have this same skin pattern.The National Psoriasis Foundation defines moderate psoriasis as covering 3-10% of your body surface. Severe means more than 10%. That’s not just a cosmetic issue. It can burn, itch, crack, and bleed. For many, it’s not just physical-it’s emotional. People report feeling stared at, judged, or even avoided. That’s why treating psoriasis isn’t just about creams. It’s about restoring confidence, too.
When Psoriasis Turns Into Joint Pain
About 30% of people with psoriasis eventually develop psoriatic arthritis. For most-85%-the skin comes first. But in 5-10% of cases, the joints hurt before the rash appears. That’s when things get tricky. Doctors might miss it, thinking it’s regular arthritis or a sports injury.Patient stories often start with stiff fingers in the morning. Swollen toes that feel like they’re stuffed in socks. Aching lower back that doesn’t improve with rest. These aren’t normal aches. They’re signs of inflammation. One hallmark is dactylitis-whole fingers or toes puffing up like sausages. It happens in about 40% of PsA cases. Another is enthesitis, where tendons pull away from bones. The Achilles tendon and bottom of the foot are common spots. That’s why some people say walking feels like stepping on gravel.
And then there’s the nails. Eight out of ten people with PsA get nail changes. Pitting. Thickening. The nail lifting off the bed. These aren’t fungal infections. They’re direct signs of immune activity. If you’ve had psoriasis for years and now your nails look strange, don’t ignore it.
How Doctors Diagnose Psoriatic Arthritis
There’s no single blood test for PsA. That’s why diagnosis relies on a mix of clues. Doctors use the CASPAR criteria, developed in 2006 and still the gold standard. To confirm PsA, you need inflammatory joint disease plus at least three of these:- Current psoriasis (3 points)
- History of psoriasis (2 points)
- Nail changes (1 point)
- Negative rheumatoid factor (1 point)
- Characteristic bone changes on X-ray (1 point)
A score of 3 or more means PsA. The system is 91.4% sensitive and 99.1% specific-meaning it rarely misses or mislabels.
Testing includes blood work for inflammation markers like CRP and ESR. X-rays show bone erosion in 60-70% of established cases. MRIs and ultrasounds catch early changes before they show on X-rays. Skin biopsies help rule out eczema or fungal infections. Family history matters too-about 40% of PsA patients have a close relative with psoriasis or arthritis.

What’s Happening Inside Your Body?
Your immune system is supposed to protect you. In PsA, it goes rogue. Genetic risks play a big role. Certain HLA genes-like HLA-B27, HLA-B38, and HLA-B39-make you more likely to develop it. But genes alone don’t cause it. Something triggers it. Stress. Infection. Injury. Even gut bacteria.Recent research points to the gut-skin-joint axis. People with PsA have different gut microbes than those without it. That imbalance might be fueling inflammation. It’s why some doctors now recommend dietary changes alongside medication.
The inflammation doesn’t stop at skin and joints. It’s systemic. That’s why PsA is linked to heart disease, diabetes, and depression. Up to 50% of patients have metabolic syndrome. Their risk of heart attack is 43% higher than the general population. Depression hits 20-30% of people with PsA. Quality of life scores are 30-40% lower than healthy peers.
Treatment: From Pain Relief to Stopping Damage
The goal isn’t just to feel better today. It’s to stop joint damage before it’s permanent. Treatment follows a step-by-step approach.For mild cases, NSAIDs like ibuprofen help with pain and swelling. But they don’t stop the immune attack. That’s where DMARDs come in. Methotrexate, taken weekly, slows disease progression for many. But for moderate to severe PsA, biologics are game-changers.
These are injectable or IV drugs that block specific inflammation signals:
- TNF inhibitors (adalimumab, etanercept): Work well for joint pain and back stiffness. Reduce ACR20 response in 50-60% of patients.
- IL-17 inhibitors (secukinumab, ixekizumab): Best for skin plaques. Clear skin faster than TNF blockers.
- IL-12/23 inhibitors (ustekinumab): Good for both skin and joints.
- JAK inhibitors (tofacitinib): Oral pills that block internal inflammation signals.
According to the American College of Rheumatology, treatment choice depends on where the disease hits hardest. If your back is stiff, go with a TNF inhibitor. If your skin is flaring, IL-17 blockers are often better.
The new target? Minimal Disease Activity (MDA). That means:
- Tender joints ≤1
- Swollen joints ≤1
- Psoriasis covers ≤1% of skin
- Pain score ≤15/100
- Global health score ≤20/100
- HAQ disability score ≤0.5
- No fatigue
Reaching MDA isn’t easy. But it’s possible-and it changes lives.

What’s Next? The Future of PsA Care
New drugs are coming fast. Guselkumab and risankizumab target IL-23, a key driver of inflammation. Deucravacitinib, a TYK2 inhibitor, is now approved and taken as a daily pill. Bimekizumab, which blocks both IL-17A and IL-17F, shows even stronger skin clearance.Biomarkers are also getting smarter. Blood tests for calprotectin and MMP-3 might soon predict who responds best to which drug. That’s precision medicine-no more trial and error.
Imaging is improving too. High-res ultrasound and MRI can spot inflammation before it destroys bone. That means starting treatment earlier, before damage sets in.
By 2027, experts predict 70% of PsA patients will be on biologics or targeted drugs within two years of diagnosis. That’s up from 40% today. Early treatment isn’t optional anymore. It’s essential.
Living With PsA: More Than Medication
Medicine helps. But it’s not everything. Diet, movement, and mental health matter just as much.Weight loss reduces joint stress and lowers inflammation. Even 5-10% body weight loss improves symptoms. Low-impact exercise-swimming, cycling, yoga-keeps joints moving without pounding them.
Stress is a known trigger. Mindfulness, therapy, or even just talking to someone who gets it can make a difference. Support groups are powerful. You’re not alone.
And don’t forget screenings. Regular checks for blood pressure, cholesterol, and blood sugar are part of PsA care. Heart disease is the #1 killer in this group. Catching it early saves lives.
Psoriasis and psoriatic arthritis are lifelong. But they don’t have to define you. With the right care, most people live full, active lives. The key? Don’t wait. If your skin is flaring and your joints are stiff, see a rheumatologist. Don’t let it be ‘just aging.’ It might be your immune system screaming for help.
Can psoriasis cause joint damage even if I don’t feel much pain?
Yes. Inflammation can quietly damage joints before pain becomes noticeable. Many people with psoriatic arthritis have early joint changes visible on MRI or ultrasound, even when they feel fine. That’s why regular checkups with a rheumatologist are critical-even if symptoms seem mild.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis (RA) is a different autoimmune disease. RA typically affects small joints symmetrically and tests positive for rheumatoid factor. Psoriatic arthritis often affects fingers asymmetrically, causes dactylitis and enthesitis, and is usually rheumatoid factor negative. The treatments overlap, but the underlying causes and patterns are distinct.
Can diet cure psoriatic arthritis?
No diet can cure it. But some people find that reducing sugar, processed foods, and alcohol helps lower inflammation. Omega-3 fatty acids from fish and anti-inflammatory foods like leafy greens may improve symptoms. Weight loss, especially, can reduce joint stress and improve medication response. Diet supports treatment-it doesn’t replace it.
Does psoriatic arthritis get worse with age?
Not necessarily. PsA doesn’t automatically worsen over time. But without treatment, joint damage can accumulate. The key is early, consistent care. Many people who start biologics early stop disease progression entirely. Age isn’t the enemy-delayed treatment is.
Are biologics safe for long-term use?
Biologics are generally safe for long-term use under medical supervision. They do increase the risk of infections slightly, so screening for TB and hepatitis before starting is standard. Regular monitoring helps catch issues early. For most, the benefits-preventing joint damage, improving mobility, reducing pain-far outweigh the risks.
Can I still exercise with psoriatic arthritis?
Yes-and you should. Movement keeps joints flexible and reduces stiffness. Low-impact activities like swimming, cycling, tai chi, and yoga are ideal. Avoid high-impact sports during flares. Physical therapists can design safe routines tailored to your joint involvement. Staying active helps control weight, reduces inflammation, and boosts mood.
Alex Curran
December 19, 2025 AT 17:57Been living with psoriasis since I was 16 and PsA since 28. The nail pitting was the first red flag no one took seriously. Got diagnosed after my pinky finger swelled up like a sausage during a hike. Doctors thought it was a sports injury. Took six months to get the right referral. Now on secukinumab and my skin is clear. Joints still ache sometimes but I can hold my kid without wincing. Don't ignore the small stuff.
Lynsey Tyson
December 20, 2025 AT 10:17My mom had this and she never talked about it. Just wore long sleeves all summer and never showed her hands. I didn't realize how much pain she was in until I got diagnosed too. It's weird how something that looks like just skin can wreck your whole life. I started yoga last year and it helped more than I expected. Not a cure but it gives me back some peace.
Edington Renwick
December 21, 2025 AT 01:45Look I'm not saying the pharmaceutical industry isn't profiting off this but why are we all just accepting these billion-dollar biologics as the only answer? I've seen people go bankrupt just to stay on their meds. And don't get me started on the 'gut-skin-joint axis' nonsense. It's all just trendy buzzwords to sell more tests and injections. Real healing is about detoxing and eating clean. Why isn't anyone talking about that?
Sarah McQuillan
December 21, 2025 AT 10:52Okay but have you heard about the CDC's secret program to track psoriasis patients through their Walmart loyalty cards? I'm not joking. My cousin works at a clinic and she says they're feeding data to Big Pharma so they can target ads for biologics based on your grocery purchases. Also why is everyone so quick to blame the gut? What about the 5G towers? I read a guy on Reddit who said his PsA cleared up after he wrapped his house in aluminum foil. Coincidence? I think not.
Aboobakar Muhammedali
December 22, 2025 AT 12:26I come from a small town in India where no one even knows what psoriatic arthritis is. My uncle had it for 20 years and they thought it was just arthritis from working too hard. He couldn't hold his grandkids. When I finally got him to a specialist in Delhi, they told him he'd lost 60% of cartilage in his knees. I cried for three days. Now he's on methotrexate and he can walk again. I just want people to know it's not rare. It's just invisible until it's too late.
Laura Hamill
December 23, 2025 AT 12:23OMG I JUST FOUND OUT MY NEIGHBOR HAS PSORIASIS AND SHE NEVER TOLD ME 😱 I THOUGHT SHE WAS JUST DRY SKIN BUT NOW I'M SCARED SHE'S GOING TO SPREAD IT TO MY CAT 😭
Alana Koerts
December 24, 2025 AT 03:51Biologics are overhyped. The data is cherry-picked. Most patients still have flares. And the cost? Ridiculous. If you're not rich, you're just being told to suffer longer. Also, the gut theory is just a distraction. The real cause is environmental toxins. Nobody talks about that because it implicates the government and corporations. Wake up.
Dikshita Mehta
December 25, 2025 AT 08:39One thing the article doesn't mention enough is how important physical therapy is. I had a PT who specialized in autoimmune conditions and she taught me how to move without aggravating my joints. Simple things like using a cane on the opposite side of my stiff knee made a huge difference. Also, staying active doesn't mean running marathons. It means moving every day-even if it's just stretching while watching TV. Small habits add up.
pascal pantel
December 26, 2025 AT 15:55Let's be real. The CASPAR criteria are outdated. They're based on 2006 data. We now have high-res imaging, cytokine profiling, and AI-driven biomarker analysis. The fact that we're still relying on subjective joint counts and nail pitting is a systemic failure. If you're not using CRP + MMP-3 + ultrasound to guide therapy, you're practicing 1990s medicine. And yes, I've published on this. The field needs to evolve or it will keep failing patients.