Manufacturing Cost Analysis: Why Generic Drugs Are So Much Cheaper

Why does a bottle of generic ibuprofen cost $2 while the brand-name version costs $15? It’s not magic. It’s math. And the math behind generic drug production explains why 90% of all prescriptions in the U.S. are filled with generics-even though they make up less than 16% of total drug spending.
The Hidden Cost of Innovation
Branded drugs don’t come cheap. Before a single pill hits the shelf, a pharmaceutical company spends an average of $2.6 billion and 10 to 15 years developing it. That includes thousands of clinical trials, years of regulatory back-and-forth, and massive marketing campaigns to convince doctors and patients the drug is worth the price. The FDA requires full safety and efficacy data for every new chemical entity. That’s expensive. And it’s why the first brand-name drug for a condition often carries a price tag that covers not just production, but the cost of every failed drug that came before it. Generic manufacturers don’t pay that bill. They don’t need to. Thanks to the 1984 Hatch-Waxman Act, all they have to prove is that their version works the same way in the body as the original. No new clinical trials. No massive patient studies. Just bioequivalence testing-checking that the active ingredient is absorbed at the same rate and amount. That cuts development costs from billions to just $2-5 million. That’s not a discount. That’s a different game entirely.How Generic Production Actually Works
Let’s break down what goes into making a generic pill. There are four main cost buckets: Active Pharmaceutical Ingredients (API), excipients, quality control, and packaging. Of these, API is the biggest. It’s the actual medicine-the thing that treats your condition. For common drugs like metformin or atorvastatin, the API is cheap because it’s been around for decades. But even small changes in the price of raw materials can swing API costs by 20-30% a year. That’s why generic makers are always hunting for new suppliers, often in India or China, where production is cheaper. Excipients are the non-medicinal ingredients-fillers, binders, coatings-that give the pill its shape and help it dissolve. These are standardized. No one owns a patent on lactose or magnesium stearate. That means generic manufacturers can buy them in bulk from any supplier. No brand loyalty. No premium pricing. Quality control is non-negotiable. The FDA requires generics to meet the same standards as branded drugs. But here’s the catch: generic companies don’t need to do the same level of post-market surveillance. Branded drugs must track every single adverse reaction for years. Generics, once approved, have lighter reporting requirements. That saves millions. Packaging? Also standardized. A 30-count bottle of generic lisinopril looks the same as the brand version. But generic makers buy bottles, labels, and blister packs in volumes that make the per-unit cost almost negligible.Scale Is Everything
The real secret to low prices? Volume. Every time a generic manufacturer doubles its production of a single drug, the cost per unit drops by 18%. For high-volume drugs like metformin or simvastatin, that means producing billions of pills a year. When six or more companies make the same generic, prices can fall by more than 95% compared to the original brand. Take cetirizine, the generic version of Zyrtec. When the patent expired, dozens of manufacturers jumped in. Within two years, the price per pill dropped from $1.20 to $0.02. That’s a 98% drop. And that’s not rare. It’s normal. The same thing happened with fluoxetine (Prozac), ciprofloxacin (Cipro), and lansoprazole (Prevacid). Each time, the price collapsed. That’s not because the ingredients got cheaper. It’s because competition forced every manufacturer to squeeze out every penny of inefficiency. A 1% improvement in production speed can mean the difference between staying in business or going under.
Why Generics Don’t Make Much Money
You might think that with such low costs, generic makers are raking in profits. They’re not. In fact, half of their revenue goes straight to production. The rest covers overhead, compliance, and distribution. Profit margins are razor-thin-often under 10%. That’s why many generic companies are owned by bigger players like Teva or Sandoz, who spread risk across hundreds of products. And here’s the irony: the same company that makes a generic version of a drug might also own the brand version. In those cases, they’ll make 201% to 1,016% more profit selling the brand-name drug-even though the pill inside is identical. That’s why pharmacies often push branded drugs: they get paid more for them.Where Generics Struggle
Not all drugs are easy to copy. Complex formulations like inhalers, injectables, or transdermal patches require advanced manufacturing tech and strict environmental controls. These are called “complex generics.” They’re harder to produce, harder to test, and harder to get approved. That means fewer companies can make them-and prices stay higher. For example, generic versions of asthma inhalers still cost 3-5 times more than simple oral pills. Why? Because the aerosol delivery system is patented separately. Even if the drug is off-patent, the device isn’t. That’s a loophole that keeps prices up. Also, when a drug has only one or two generic makers, prices don’t drop as much. FDA data shows that with just two competitors, generics are only 54% cheaper than the brand. But with six or more? That’s when prices really crash.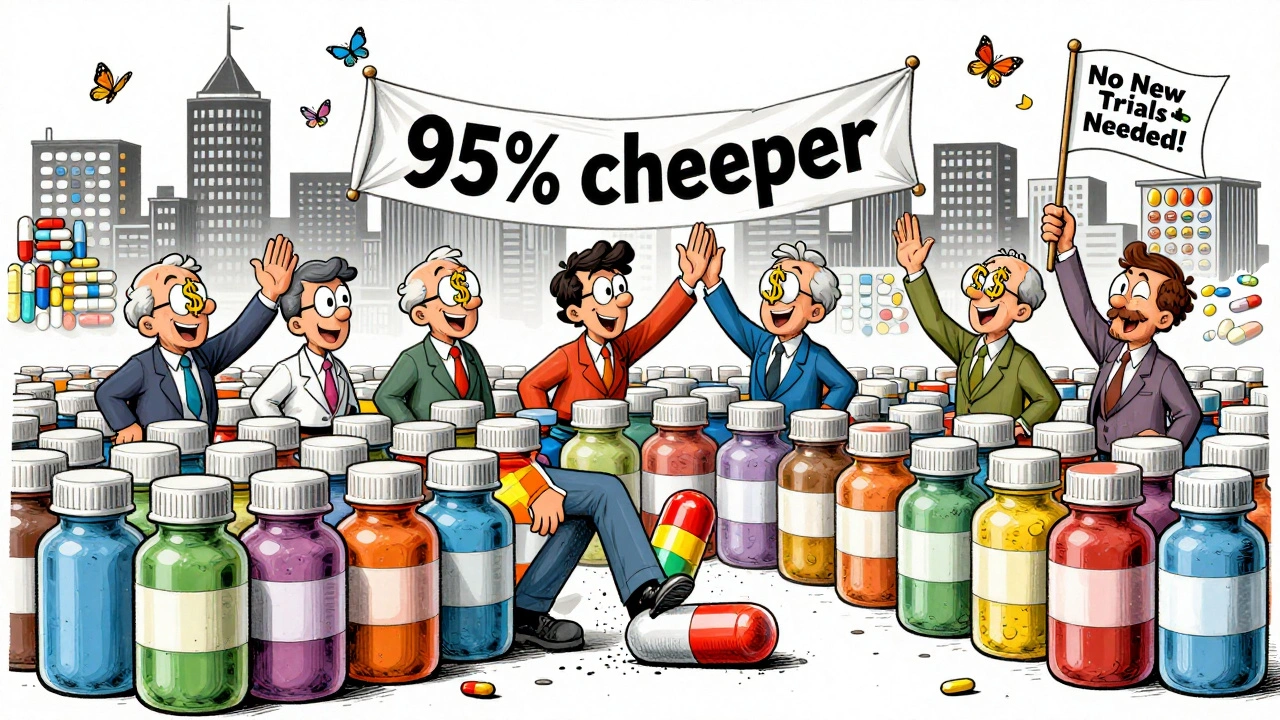
Jim Irish
December 11, 2025 AT 10:16Generics are the unsung heroes of healthcare
People act like they're inferior but the FDA makes them prove they're identical
Same active ingredient, same absorption, same results
Just no marketing budget and no R&D debt
That's all it takes
Kristi Pope
December 11, 2025 AT 16:13I love how generics let grandma afford her blood pressure meds without choosing between pills and groceries
It’s not just about savings-it’s about dignity
And honestly? The pill in that $2 bottle works just as well as the $15 one
Why do we still act like brand names are magic?
Aman deep
December 13, 2025 AT 02:35as a guy from india where many api are made
we see this every day
small factories run 24/7 with workers who know every step
the cost is low because labor is cheap and scale is huge
but quality? its not always perfect
some batches get rejected by fda
but most? they’re solid
we just dont talk about the mess behind the bottle
Vivian Amadi
December 13, 2025 AT 23:06Oh please. You think generics are ‘smart’? They’re parasites
They ride on the backs of companies that spent billions
Then they undercut them to the point where innovation dies
You want cheap pills? Fine
But when the next cancer drug never gets made because no one can afford to develop it-you’ll thank me
matthew dendle
December 15, 2025 AT 09:03generic makers be like ‘we dont need no stinkin’ trials’
branded pharma be like ‘we spent 15 years and 2.6 bil’
then the same company sells both and makes 10x more on the brand
so who’s the real scammer here? hmmmm
Taylor Dressler
December 15, 2025 AT 15:25There’s a common misconception that generics are ‘lesser’-but the bioequivalence standards are strict. The FDA requires the 90% confidence interval for AUC and Cmax to fall within 80–125% of the brand. That’s not luck. That’s science.
And yes, packaging is standardized-but so is the active ingredient’s purity. Every batch is tested. Every lot is tracked.
The real difference isn’t quality. It’s marketing. And that’s why the system works.
Jean Claude de La Ronde
December 15, 2025 AT 18:09So we’ve optimized pills to the point where profit margins are thinner than a placebo
Meanwhile, the same corporations that make generics also own the brand names
And they charge 10x for the same molecule
Is this capitalism? Or just a really well-designed con?
At what point do we stop calling it ‘free market’ and start calling it ‘legalized extortion’?
Mia Kingsley
December 17, 2025 AT 10:45you think this is about cost? no its about control
big pharma lets generics exist so people think they’re saving money
but then they own the patents on the machines that make the pills
and the packaging suppliers
and the shipping contracts
and the pharmacies that push the brand
you’re not saving money
you’re just being tricked into thinking you are
Courtney Blake
December 17, 2025 AT 13:03USA should ban all foreign API. End of story.
India and China are playing us. We’re dependent on them for our meds.
What if war breaks out? What if they cut supply?
We’re literally letting our health be held hostage by dictators and corrupt factories.
Fix this now or we’ll all be dead by 2030 💀