How to Create a Medication Plan Before Conception for Safety

Planning for pregnancy isn’t just about taking prenatal vitamins or tracking ovulation. If you’re on any medication - even over-the-counter pills, supplements, or herbal remedies - your body needs time to adjust before conception. Why? Because the most critical window for fetal development happens before you even know you’re pregnant. Major organs like the heart, brain, and limbs form between weeks 3 and 8. By the time a home pregnancy test turns positive, that window is already closing. That’s why a preconception medication plan isn’t optional - it’s essential.
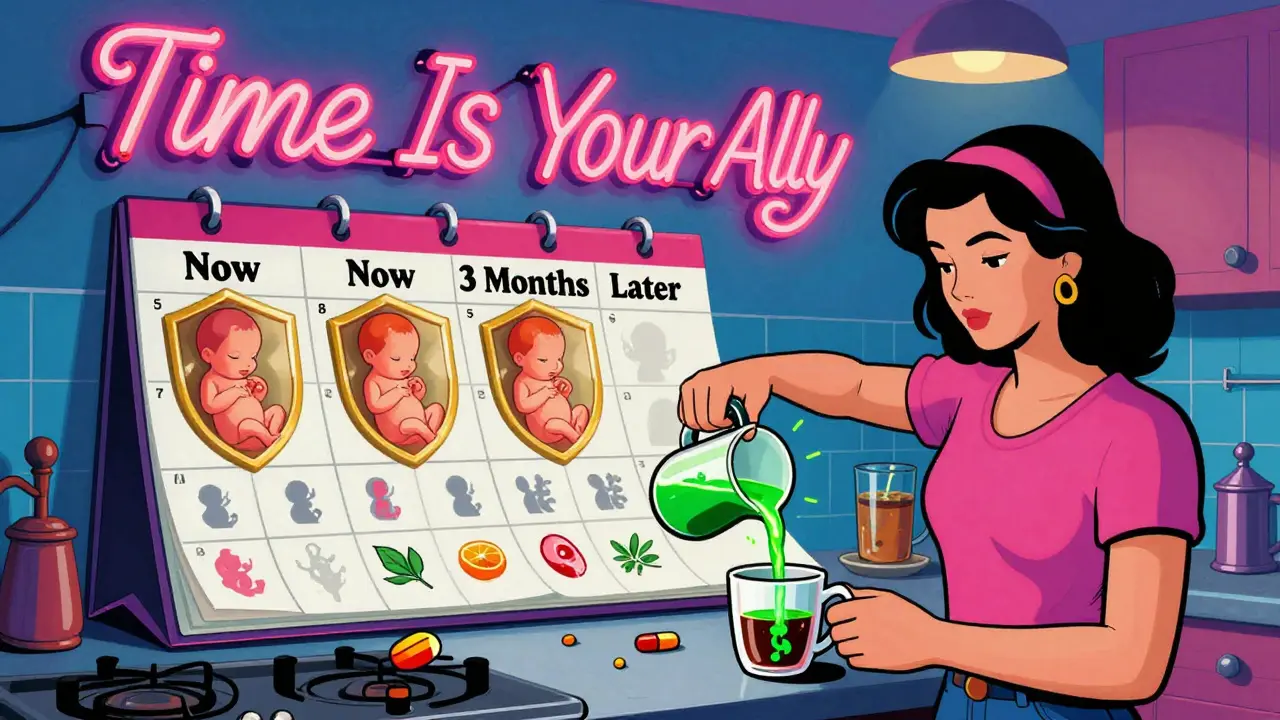
Why Timing Matters More Than You Think
Most women don’t realize they’re pregnant until after week 4 or 5. But by then, the embryo has already started forming its spine, eyes, and heart. If you’re taking a drug that can cross the placenta - like certain seizure meds, acne treatments, or mood stabilizers - you could be exposing your baby to risks without ever knowing it. According to the American College of Obstetricians and Gynecologists (ACOG), nearly half of all pregnancies in the U.S. are unplanned. That means a lot of women are unknowingly taking medications during this sensitive period. The good news? You can prevent most of these risks if you plan ahead.What Medications Should You Review?
Don’t just think about prescription drugs. Your preconception checklist should include:- All prescription medications (even for chronic conditions like epilepsy, diabetes, or depression)
- Over-the-counter painkillers (like ibuprofen or naproxen)
- Supplements (vitamins, fish oil, herbal teas)
- Acne treatments (especially isotretinoin)
- Thyroid meds, blood thinners, and immunosuppressants
Folic Acid: The One Supplement Everyone Needs
Folic acid isn’t just for women with high-risk pregnancies. It’s for every woman of childbearing age. The World Health Organization recommends 400 mcg daily for all women aged 15-49. But if you have certain conditions - like epilepsy, diabetes, or a previous baby with a neural tube defect - you need more. ACOG and the Centre for Effective Practice suggest 4-5 mg daily in those cases. Why? Because folic acid reduces the risk of spina bifida and anencephaly by up to 70%. And since neural tube closure happens by week 6, waiting until you’re pregnant to start taking it is too late.High-Risk Medications to Avoid Before Conception
Some drugs are simply too dangerous to use during early pregnancy. Here are the big ones:- Valproic acid - linked to facial deformities, heart defects, and intellectual disability
- Lithium - increases risk of Ebstein’s anomaly (a heart defect)
- Topiramate - raises risk of cleft lip/palate
- Methotrexate - causes severe birth defects and miscarriage
- Isotretinoin (Accutane) - causes skull, eye, and heart defects; requires 1 month of contraception after stopping
- Cyclophosphamide - can permanently damage ovaries

Thyroid and Blood Sugar: Hidden Risks
Many women don’t realize that uncontrolled thyroid disease or diabetes can be just as risky as dangerous medications. If your TSH (thyroid-stimulating hormone) level is above 2.5 mIU/L before pregnancy, your risk of miscarriage increases by 60%. That’s why doctors recommend adjusting your levothyroxine dose before conception - not after. Same goes for blood sugar. Women with type 1 or type 2 diabetes need to get their HbA1c below 6.5% before trying to get pregnant. High glucose levels during early pregnancy can cause heart defects, brain abnormalities, and even stillbirth.What About Mental Health Meds?
Stopping antidepressants or anti-anxiety meds might sound scary - and sometimes it is. But untreated depression during pregnancy carries its own risks: preterm birth, low birth weight, and postpartum depression. The key is choosing the right drug. SSRIs like sertraline and citalopram are considered low-risk. Avoid paroxetine - it’s linked to a slightly higher risk of heart defects. Never stop your meds cold turkey. Work with your psychiatrist and OB-GYN to taper slowly and switch if needed.How Long Before Conception Should You Start?
The gold standard? Start at least 3 to 6 months before you plan to conceive. Why? Because:- Some drugs need 3 months to fully clear (like methotrexate)
- Switching meds takes time to find the right dose
- Chronic conditions like lupus or asthma need stabilization
- Contraception may need to change - especially if you’re on seizure meds that reduce birth control effectiveness
Who Should You Talk To?
This isn’t a one-doctor job. You need a team:- Your OB-GYN - to coordinate everything
- Your specialist - neurologist, endocrinologist, psychiatrist, rheumatologist
- Your pharmacist - they know drug interactions better than anyone
What If You’re Already Pregnant?
If you just found out you’re pregnant and haven’t reviewed your meds yet - don’t panic. But don’t wait either. Call your doctor immediately. Some changes can still be made safely in early pregnancy. Folic acid can still help. Some meds can be switched. But the clock is ticking. The first 8 weeks are the most critical. Every day counts.Real-World Barriers - And How to Overcome Them
The system isn’t perfect. Only 38% of women with chronic conditions get proper preconception counseling. Why? Because doctors are busy. Insurance doesn’t always cover it. Women don’t know they need it. But here’s the thing: you don’t need to wait for the system to catch up. Take action now. Schedule a preconception visit. Bring your pill bottles. Ask your pharmacist to check for interactions. Use apps like Luma Health’s Preconception Navigator (FDA-approved since 2023) to scan your meds against teratogen databases.What’s Next?
The future of preconception care is personalized. The NIH’s PharmaTox study (launched in 2023) is testing how your genes and metabolism affect how drugs impact your baby. But right now, the best tool you have is time - and knowledge. Plan ahead. Review every pill. Talk to your team. Don’t wait for pregnancy to find you.Do I need to stop all my medications before getting pregnant?
No. Many medications are safe during pregnancy - including thyroid meds, certain antidepressants, and insulin. The goal isn’t to stop everything, but to replace risky ones with safer alternatives before conception. Always consult your doctor before making any changes.
How long before trying to conceive should I start planning?
At least 3 to 6 months. Some medications, like methotrexate or isotretinoin, require months to fully leave your system. This timeframe also allows your body to stabilize chronic conditions like diabetes or epilepsy before pregnancy.
Is folic acid really that important if I’m not planning to get pregnant?
Yes. Since nearly half of pregnancies are unplanned, the World Health Organization recommends 400 mcg of folic acid daily for all women aged 15-49. It’s a simple, low-cost way to prevent serious birth defects - even if you’re not actively trying.
Can I keep taking my anxiety or depression meds?
Many are safe. Sertraline and citalopram are considered low-risk. Paroxetine should be avoided due to a small heart defect risk. Never stop cold turkey - work with your psychiatrist to switch or adjust doses safely before conception.
What if I’m on birth control and want to get pregnant?
If you’re on hormonal birth control, you can stop it and try to conceive right away. But if you’re on seizure meds like carbamazepine, your birth control might not work well - ask your doctor about backup methods. Also, give yourself time to adjust your body before trying to conceive.