HCV Reinfection and Cure: How Retreatment and Harm Reduction Keep People Healthy

After beating hepatitis C with direct-acting antivirals (DAAs), many people think they’re done. But for some, the virus comes back. HCV reinfection isn’t rare-it’s a real and growing challenge, especially among people who still face high-risk behaviors like injecting drugs. The good news? You can be cured again. And again. And again. Treatment works, no matter how many times you get infected. What matters now isn’t whether you can be cured-it’s how we make sure you stay cured.
Why HCV Comes Back After a Cure
Hepatitis C is curable in over 95% of cases with just 8 to 12 weeks of oral medication. Since DAAs arrived in 2014, the game changed. No more injections, no more side effects like crushing fatigue or depression. Just pills. But cure doesn’t mean immunity. If you’re still injecting drugs, sharing needles, or using unsterile equipment, the virus can slip back in. Studies show the highest risk is in the first six months after treatment. Younger people under 30, those still using methamphetamine, and people who inject drugs regularly have up to 3 times the risk of reinfection.It’s not about being "bad" or "not trying." It’s about environment. If you’re living in a community with no clean needles, no safe spaces, or no access to opioid treatment, the virus will find a way back. That’s why cure alone isn’t enough. You need harm reduction to keep the virus out for good.
How Retreatment Works-And Why It’s Just as Effective
Some providers still hesitate to treat someone who’s been infected before. They think, "Why bother? They’ll just get it again." That’s outdated thinking. Data from JAMA Network Open in 2024 confirms: retreatment works just as well as the first round. Whether it’s your second, third, or fifth infection, the cure rate stays above 95% with the right drugs.The standard retreatment for reinfection is glecaprevir/pibrentasvir (Mavyret) for 8 weeks. For relapse-when the virus comes back after treatment-you might need 12 weeks of sofosbuvir/velpatasvir/voxilaprevir (Vosevi) or 16 weeks of Mavyret with ribavirin. Resistance testing is only needed if you relapsed, not if you got reinfected. That’s important: reinfection means you caught a new strain, not that the old one came back. That’s why the same treatment works again.
And now there’s a new option: 4-week treatment for early infection. The PURGE-C trial showed 84% cure rates with just 4 weeks of Mavyret for people who tested positive within 24 weeks of exposure. It’s not quite as strong as the 12-week course, but it’s close-and for someone who might disappear from care, it’s a lifeline. The NIH is already testing a 2-week version in a new trial called PURGE-2. Shorter courses mean more people get treated before they pass it on.
Harm Reduction Isn’t Optional-It’s Essential
You can’t cure your way out of an epidemic if you don’t stop the spread. That’s where harm reduction comes in. It’s not about encouraging drug use. It’s about saving lives while people work toward change.Needle and syringe programs (NSPs) that give out at least 200 clean needles per person per year cut HCV transmission by 54%. Methadone or buprenorphine (opioid agonist therapy) reduces new infections by half. These aren’t guesses-they’re proven, measurable results from global studies. Yet in 62% of countries, these programs are still banned, restricted, or underfunded.
In the U.S., 32 states now allow "treatment on demand" for people who inject drugs. That means you can walk into a clinic, get tested, and start HCV treatment the same day-no waiting, no judgment. But here’s the problem: only 1 in 5 people who need it actually get access. Too many clinics still refuse treatment because someone is using drugs. A 2024 survey found 68% of people who inject drugs were turned away from HCV care because of their drug use. That’s not just wrong-it’s deadly.
Integrated Care Saves Lives
The best outcomes happen when HCV treatment is tied to addiction care. In Boston, clinics that co-located hepatitis C care with medication-assisted treatment (MAT) saw 82% of patients stick with their treatment plan. Why? Because they didn’t have to jump between two separate systems-one for their liver, another for their addiction. One provider. One appointment. One team.That’s the model that works. When you treat the whole person, not just the virus, cure lasts. When you separate care, people fall through the cracks. One San Francisco study found 74% of people who relapsed struggled to navigate between addiction centers and liver specialists. They got lost in the system. And by the time they found help, the virus was back.
What You Need to Know After Treatment
Even after you’re cured, you’re not done. You need follow-up. For the first six months, get tested for HCV RNA every three months. That’s when reinfection is most likely. After that, testing every 6 to 12 months is enough if your risk is lower.Also, get tested for hepatitis B before starting HCV treatment. DAAs can wake up a dormant HBV infection. Between 2019 and 2024, 12 U.S. cases of HBV reactivation were reported during HCV treatment. It’s rare, but serious. Your doctor should check your HBV status before you take your first pill.
And remember: your immune system doesn’t bounce back fully after HCV cure. If you had advanced liver scarring (fibrosis), your T cells stay worn out. That doesn’t mean you can’t be cured again. But it does mean you need to protect your liver harder than ever. No alcohol. No risky behaviors. No delays in care.
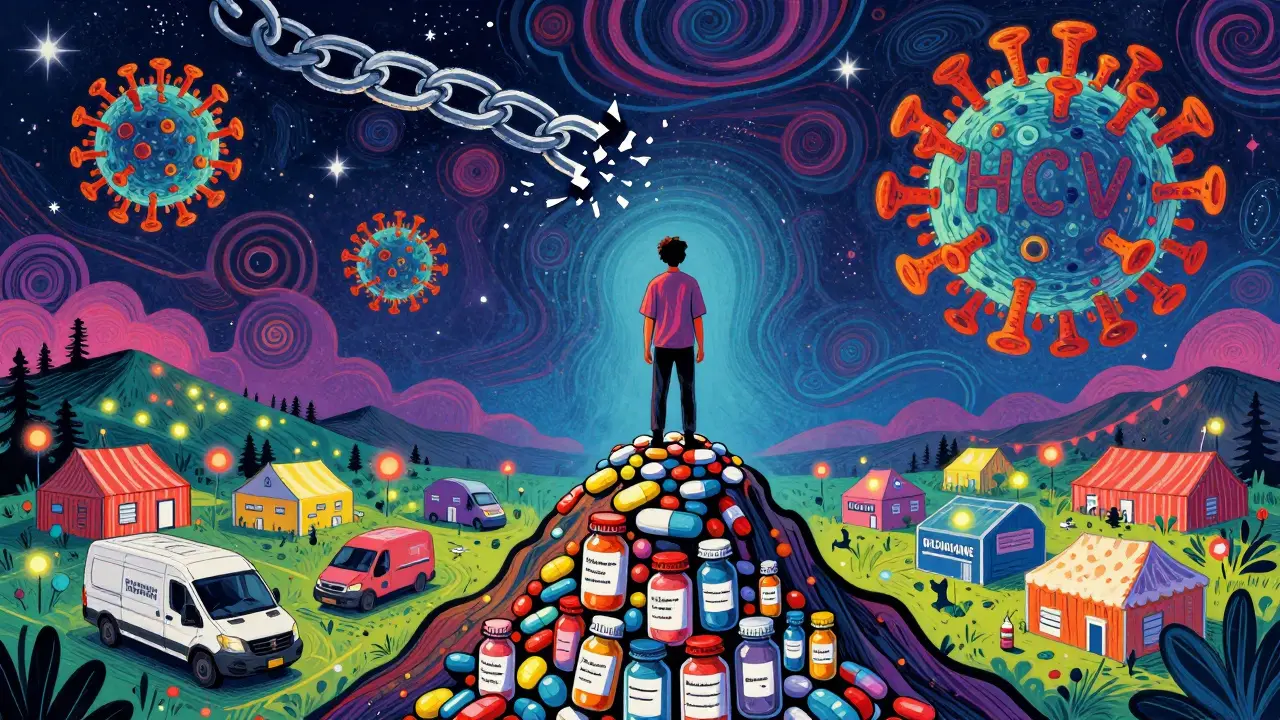
The Bigger Picture: Can We Really Eliminate HCV?
The World Health Organization wants to eliminate HCV by 2030. That means cutting new infections by 90% and treating 80% of people who have it. Right now, 58 million people live with HCV. Only 20 million have been treated. We’re moving, but not fast enough.The tools exist: cheap, effective pills. Clean needles. Opioid treatment. Same-day care. But political will is missing. Funding is uneven. Stigma is still the biggest barrier. People who inject drugs are told to "get clean" before they get treated. But we know that’s backwards. Treatment helps people get clean. It gives them stability, hope, a reason to care for their body.
Models show we can hit the 2030 goal-if we treat at least 15% more people every year and cover more than 60% of people who inject drugs with clean needles. That’s doable. But only if we stop treating people like problems and start treating them like patients.
What This Means for You
If you’ve been cured and you’re still at risk, don’t wait for the next infection to seek help. Get tested every few months. Use clean needles. Talk to your provider about methadone or buprenorphine if you’re using opioids. Ask about same-day treatment programs. You don’t need to be perfect to deserve care. You just need to be alive.If you’re a provider: treat every person, every time. No exceptions. No waiting. No stigma. The science is clear: cure is possible, repeatable, and life-saving. Your job isn’t to judge who deserves it. It’s to make sure they get it.
Hepatitis C doesn’t care if you’ve been cured before. It only cares if you’re exposed. But you do have power. You can choose clean needles. You can choose treatment. You can choose to keep coming back-even if you’ve been turned away before. Because every time you do, you’re one step closer to staying cured for good.
Stephen Craig
January 5, 2026 AT 04:37Reinfection isn't failure. It's a symptom of systems that fail people. Cure is easy. Care is hard.
Jason Stafford
January 6, 2026 AT 22:29They’re lying about the cure rates. DAAs were designed by Big Pharma to keep people coming back for more. You think they want you cured? They want you dependent. Look at the patents. Look at the pricing. This isn’t medicine-it’s a cash grab disguised as compassion.
Charlotte N
January 7, 2026 AT 08:27so like… if you get cured and then use dirty needles again… you just… get cured again?? no big deal??
Allen Ye
January 9, 2026 AT 07:56What we’re really talking about here isn’t virology-it’s moral philosophy. We’ve built a healthcare system that equates worth with compliance. If you’re not sober, you’re not worthy of care. But HCV doesn’t care about your choices-it only responds to your access. The virus is neutral. Our judgment isn’t. We treat people like problems to be managed rather than humans to be supported. That’s the real infection. Not the virus. The stigma. And it’s more contagious than any strain of HCV. We’ve created a culture where being cured is celebrated, but being at risk is punished. That’s not public health. That’s punishment dressed in white coats. We need to stop asking if someone deserves care and start asking how we can deliver it. The data doesn’t lie: harm reduction saves lives. But our policies? They’re still stuck in the 1980s. Shame isn’t a treatment modality. Compassion is. And compassion requires us to show up-even when it’s messy. Even when it’s inconvenient. Even when the person sitting across from us is still using. Because they’re not a statistic. They’re someone’s child. Someone’s sibling. Someone who just wants to live without fear of their own liver failing. And if we can cure them five times, we can damn well make sure they’re not left alone after the sixth.
Justin Lowans
January 9, 2026 AT 08:35The science is unequivocal: retreatment efficacy remains above 95% across all reinfection scenarios. The barrier is not medical-it is institutional. Clinics that require abstinence prior to treatment are not only contradicting evidence-based guidelines, they are perpetuating systemic neglect. Integrated care models, such as those implemented in Boston and San Francisco, demonstrate that co-locating hepatitis C treatment with opioid agonist therapy increases adherence by over 80%. This is not theoretical-it is operational, scalable, and cost-effective. The challenge lies not in the availability of therapeutics, but in the willingness of institutions to dismantle bureaucratic gatekeeping. We must shift from a punitive paradigm to a public health framework. Every delay in treatment is a missed opportunity to interrupt transmission. Every refusal of care is a death sentence waiting to be written.
Connor Hale
January 10, 2026 AT 20:47It’s wild how we’ll give someone a new liver but won’t give them clean needles. We fix the damage but refuse to stop the leak.
Jack Wernet
January 12, 2026 AT 13:27There is a profound moral clarity in treating patients without condition. To withhold care based on behavior is not medicine-it is moral arrogance masquerading as prudence. The physician’s oath does not include a clause for judging lifestyle. It demands healing. And healing requires presence, not perfection.
melissa cucic
January 12, 2026 AT 23:47I’ve seen this play out in rural clinics-people get cured, go home, and six months later come back with the same virus. Why? Because there’s no one to check on them. No peer support. No transportation. No harm reduction outreach. We give them pills and send them off like the problem is solved. But the problem isn’t the virus-it’s the isolation. We need case managers. We need outreach workers. We need people who show up, not just prescriptions.
Oluwapelumi Yakubu
January 14, 2026 AT 01:34Listen, in Nigeria, we don’t have DAAs in most places, but we still fight HCV with community health workers going door to door with test kits. You think it’s about pills? No. It’s about trust. When someone believes you care more than you judge, they show up. That’s the real cure. Not the drug. The connection.
Roshan Aryal
January 14, 2026 AT 07:01Why is it that every time someone says ‘harm reduction,’ someone else screams ‘enabling’? You don’t enable someone by giving them a needle. You enable them by telling them they’re not worth saving.
Joseph Snow
January 15, 2026 AT 11:054-week treatment? That’s a gimmick. They’re rushing this because they know people will stop showing up. You can’t cure addiction with a pill. You need jail time, not a prescription. This whole system is built on lies and taxpayer money.
Abhishek Mondal
January 16, 2026 AT 17:57Western countries spend billions on pills but won’t fund needle exchanges? What a joke. In India, we have over 1000 community-based HCV screening camps in slums-no ID, no insurance, no judgment. You want to eliminate HCV? Stop pretending poverty is a choice. Start treating people like humans.
Michael Rudge
January 18, 2026 AT 09:16So let me get this straight-after you get cured, you’re supposed to just… keep using drugs? And the system is supposed to keep bailing you out? What’s next? Free insulin for diabetics who keep eating donuts? This isn’t healthcare. It’s a subsidy for self-destruction.