GLP-1s for PCOS and Obesity: Real Weight Loss and Metabolic Results

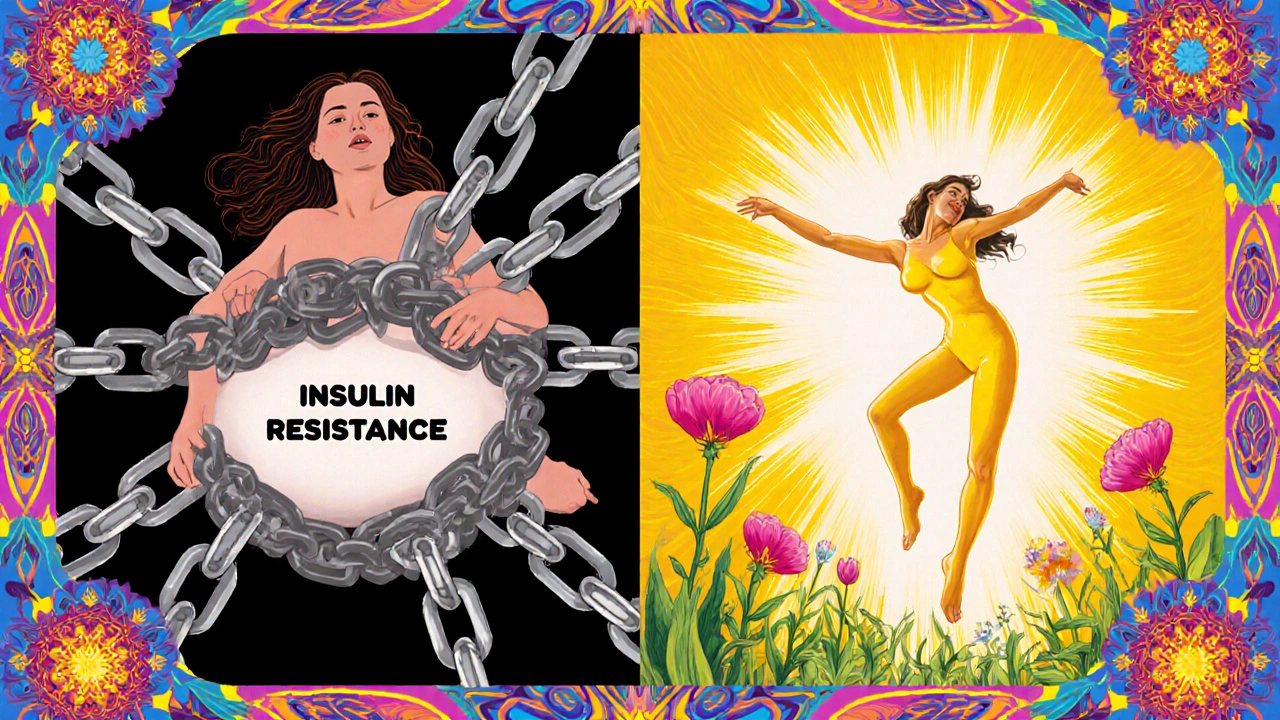
Women with PCOS often struggle with more than just irregular periods or acne. For many, the biggest challenge is weight - and not just any weight, but stubborn fat that sticks around no matter how much they diet or exercise. That’s because PCOS isn’t just a reproductive issue. It’s a metabolic disorder. Insulin resistance, high testosterone, and excess belly fat go hand in hand. And until now, the go-to treatments - metformin, birth control pills - only partly helped. Enter GLP-1 receptor agonists. These aren’t new drugs, but they’re finally being seen as game-changers for women with PCOS who are overweight or obese.
How GLP-1s Actually Work in the Body
GLP-1s mimic a hormone your gut makes after eating. That hormone tells your pancreas to release insulin only when blood sugar is high - no guessing, no crashes. It also slows down how fast food leaves your stomach. That’s why you feel full longer. But here’s the part most people miss: GLP-1s cross the blood-brain barrier. They talk directly to your appetite center. Not just "eat less," but "you don’t want to eat right now." It’s not willpower. It’s biology.
For women with PCOS, this matters because their bodies are stuck in a loop: high insulin → more fat storage → more insulin resistance → worse PCOS symptoms. GLP-1s break that loop. They don’t just help you lose weight. They lower insulin, reduce testosterone, and shrink visceral fat - the kind that wraps around your organs and raises heart disease risk.
Weight Loss Numbers You Can Trust
Let’s talk numbers. In clinical trials, women with PCOS using liraglutide (1.8-3.0 mg daily) lost about 5-10% of their body weight in 6 months. That’s not small. Losing just 5% of your weight can bring back periods, improve ovulation, and lower testosterone by 20-30%. One woman in a 2022 study went from having no period for three years to ovulating naturally after 24 weeks on liraglutide.
Semaglutide, the stronger version, does even more. In the STEP-PCOS trial, women on semaglutide 2.4 mg lost 10.2% of their body weight in just 36 weeks. Compare that to the placebo group, who lost only 2.1%. That’s not a fluke. In another study, semaglutide cut visceral fat by 18% - the kind of fat linked to diabetes and heart disease. These aren’t cosmetic changes. They’re metabolic repairs.
And it’s not just weight. In the same studies, fasting insulin dropped by 30-40%, triglycerides fell, and HDL (the good cholesterol) went up. One study showed 42% of women on liraglutide started ovulating spontaneously. That’s the kind of result doctors used to only see after bariatric surgery.
GLP-1s vs. Metformin: The Real Comparison
Metformin has been the standard for years. It helps with insulin resistance, and some women lose 2-5% of their weight on it. But for many, that’s not enough. GLP-1s don’t just beat metformin - they leave it behind in weight loss.
Studies show liraglutide leads to nearly double the weight loss of metformin in PCOS patients. Semaglutide? It’s even more dramatic. In the STEP 5 trial (for obesity without PCOS), semaglutide 2.4 mg led to 14.9% weight loss over 68 weeks. Metformin? Around 3-5%. The difference isn’t close.
But here’s the catch: metformin costs $10-$20 a month. Brand-name semaglutide (Wegovy) or liraglutide (Saxenda) can run $800-$1,400 a month. That’s why many women stay on metformin - not because it’s better, but because they can’t afford the alternative.
Side Effects: What No One Tells You
Yes, GLP-1s work. But they’re not magic. About 44% of users get nausea. A quarter get vomiting. Dizziness, fatigue, and constipation are common, especially in the first few weeks. That’s why doctors start you on a low dose - 0.25 mg weekly for semaglutide - and slowly increase it over 4-5 months.
Some women can’t tolerate it. On Reddit’s r/PCOS forum, one user wrote: "Spent $1,200 a month on Wegovy for 4 months. Lost 15 lbs. Couldn’t keep food down. Switched back to metformin." That’s real. Discontinuation rates in trials are 15-20%. It’s not failure. It’s biology. Your gut doesn’t like the sudden change.
There are also rare but serious risks. These drugs are not safe if you or a family member has had medullary thyroid cancer. They’re also not approved for use in lean PCOS patients - the ones who aren’t overweight. For them, GLP-1s offer little benefit. They’re designed for metabolic dysfunction, not just weight.
Who Benefits Most - And Who Doesn’t
GLP-1s work best for women with PCOS who have a BMI over 30 and signs of insulin resistance - high fasting insulin, prediabetes, or fatty liver. If you’re under 150 lbs and your blood sugar is normal, don’t expect much. The drugs target metabolic dysfunction, not just fat.
They’re also not for everyone long-term. If you stop taking them, most people regain weight - fast. Studies show 60-70% of women regain all the weight they lost if they stop both GLP-1s and metformin. But here’s the hopeful part: if you keep taking metformin after stopping the GLP-1, you only regain about one-third of the weight. That’s why doctors now recommend combining them.
And while GLP-1s aren’t approved yet for PCOS in most countries, that’s changing. In June 2024, the European Medicines Agency accepted Novo Nordisk’s application to approve semaglutide 2.4 mg specifically for women with PCOS and metabolic issues. A decision is expected in early 2025. That could change everything.
What to Expect When You Start
If you and your doctor decide to try a GLP-1, here’s what actually happens:
- You start with the lowest dose - usually 0.25 mg of semaglutide once a week.
- You inject it under your skin (abdomen, thigh, or upper arm). No needles, just a tiny pen.
- You wait 4 weeks, then increase the dose - slowly. Most people don’t reach the full dose until 16-20 weeks.
- Nausea hits around week 2-4. Eat smaller meals. Skip greasy food. Drink ginger tea. Most people get used to it.
- By month 3, you start noticing less hunger. Snacks don’t feel as urgent. Your clothes feel looser.
- At 6 months, you’re likely 5-10% lighter. Your periods may be regular. Your skin might clear up. Your energy improves.
Track your progress with blood tests - fasting insulin, testosterone, HbA1c. Don’t just rely on the scale. These markers tell you if your metabolism is healing.
The Future: What’s Coming Next
Oral GLP-1s are on the way. Rybelsus is already approved for diabetes, but it’s not yet used for PCOS. If it works as well as the injections, adherence will jump. No more needles. No more monthly costs from pharmacies that don’t stock them.
Even better, new drugs are in trials - triple agonists that hit GLP-1, GIP, and glucagon receptors at once. Early data shows up to 20% weight loss. That’s bariatric surgery territory, without surgery.
By 2027, experts predict GLP-1s will be standard care for obese women with PCOS - if insurance covers them. Right now, access is uneven. In Australia, Medicare doesn’t cover them for PCOS. In the U.S., some private plans do. In Europe, approval is coming fast.
This isn’t a fad. It’s the first real treatment that targets the root cause of weight gain in PCOS - not just the symptoms. For women who’ve tried everything and still gained weight, this might be the break they’ve been waiting for. But it’s not simple. It’s expensive. It’s not for everyone. And it’s not a cure.
It’s a tool. And like any tool, it only works if it’s used the right way - with the right support, the right expectations, and the right plan.
Do GLP-1s help with PCOS symptoms beyond weight loss?
Yes. Studies show GLP-1s reduce testosterone levels by 20-30%, improve menstrual regularity, and increase spontaneous ovulation in up to 42% of women after 6 months. They also lower insulin resistance, reduce liver fat, and improve cholesterol - all key metabolic issues in PCOS.
How long does it take to see results with GLP-1s for PCOS?
Most women notice reduced hunger and slight weight loss within 2-4 weeks. Noticeable changes - like looser clothes or more regular periods - usually appear between 3-6 months. Full metabolic improvements, including insulin and testosterone drops, take 6-12 months.
Can I take GLP-1s if I’m not overweight?
Probably not. GLP-1s are most effective in women with PCOS who have a BMI over 30 and signs of insulin resistance. Lean PCOS patients without metabolic issues don’t typically benefit from weight loss drugs. Treatment for them focuses on insulin sensitizers like metformin or hormonal therapies.
Are GLP-1s safe for long-term use in PCOS?
Long-term data beyond 2 years is still limited, but no new safety signals have emerged in trials lasting up to 3 years. The main concerns are gastrointestinal side effects and weight regain after stopping. They’re not recommended for people with a personal or family history of medullary thyroid cancer.
Will insurance cover GLP-1s for PCOS?
Currently, most insurance plans only cover GLP-1s for obesity or type 2 diabetes - not specifically for PCOS. Since PCOS isn’t yet an approved indication, coverage is inconsistent. Some plans approve it off-label if you have prediabetes or a BMI over 30. Always check with your provider and ask for prior authorization.
Can I combine GLP-1s with metformin?
Yes, and it’s often recommended. Combining metformin with a GLP-1 RA leads to better weight maintenance after stopping the GLP-1. One study found women who stayed on metformin after stopping semaglutide regained only one-third of their lost weight over two years - compared to 60-70% regain if they stopped both.
Jeff Hicken
November 24, 2025 AT 11:48Vineeta Puri
November 25, 2025 AT 07:35Victoria Stanley
November 26, 2025 AT 01:29Andy Louis-Charles
November 27, 2025 AT 02:22Douglas cardoza
November 27, 2025 AT 20:26Adam Hainsfurther
November 28, 2025 AT 14:43Rachael Gallagher
November 30, 2025 AT 11:55steven patiño palacio
December 1, 2025 AT 11:05stephanie Hill
December 1, 2025 AT 11:10Akash Chopda
December 2, 2025 AT 00:22Nikki C
December 2, 2025 AT 08:40Alex Dubrovin
December 4, 2025 AT 08:09