Fluticasone Allergy Management: Daily Routine Guide

Fluticasone Symptom Tracker
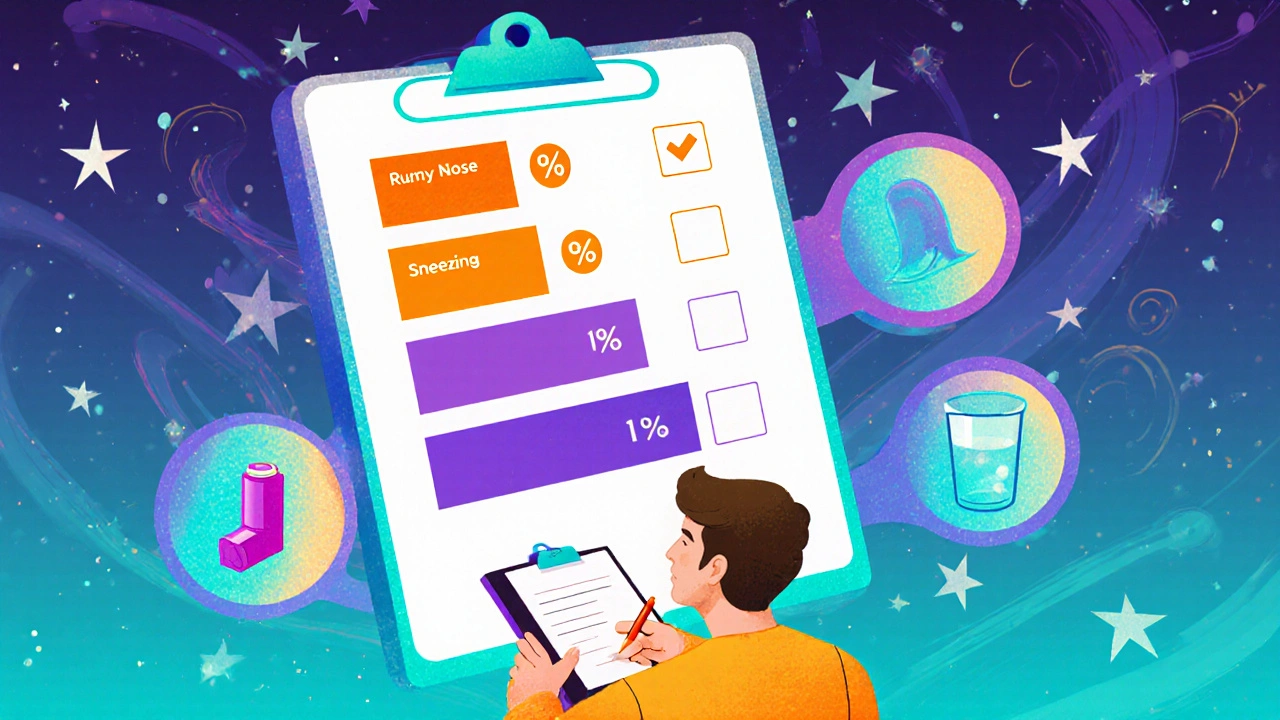
Daily Symptom Tracking
Track your symptoms for two weeks to monitor how well Fluticasone is working for your allergies.
Symptom History
| Date | Runny Nose | Sneezing | Wheeze | Improvement |
|---|---|---|---|---|
| No data yet | - | - | - | - |
How to Interpret Your Results
Effective Treatment: Symptoms should gradually decrease over 1-2 weeks. If scores drop steadily, your Fluticasone dose is likely working well.
Adjustments Needed: If symptoms don't improve after two weeks, contact your healthcare provider to discuss changing the dosage or trying additional treatments.
Side Effects: Watch for nasal dryness, nosebleeds, or throat irritation. Persistent symptoms may indicate overuse.
When tackling seasonal allergies, Fluticasone is a synthetic corticosteroid that reduces inflammation in the nasal passages and airways. It’s available in several formats, from nasal sprays to inhalers, and can fit neatly into a busy day if you know how to plan it. Below is a step‑by‑step plan that shows where Fluticasone belongs in a comprehensive, everyday allergy‑control strategy.
Understanding Fluticasone and Its Role in Allergy Management
Fluticasone works by calming the immune response that causes swelling, mucus, and itchiness. Unlike oral antihistamines, which block histamine receptors, Fluticasone targets the underlying inflammation, making it a front‑line tool for both Allergic Rhinitis inflammation of the nasal lining triggered by allergens like pollen or dust mites and mild Asthma a chronic airway disease where inflammation leads to wheezing and shortness of breath. Because it’s applied locally (nose or lungs), systemic side effects stay low, which is why doctors often recommend it for daily use.
Key attributes of Fluticasone:
- Class: Corticosteroid
- Typical dose: 50‑200 µg per spray or inhalation, depending on formulation
- Onset of action: 12‑24 hours for nasal spray, 30‑60 minutes for inhaler
- Safety profile: minimal systemic absorption when used as directed
Choosing the Right Formulation
Fluticasone comes in three main delivery methods. Picking the one that matches your symptoms and lifestyle is the first step toward a smooth routine.
| Form | Typical Use | Strength (µg per actuation) | Best For |
|---|---|---|---|
| Nasal Spray | Allergic rhinitis, post‑nasal drip | 50‑100 | People who need consistent nasal relief |
| Inhaler (Metered‑Dose) | Mild persistent asthma, exercise‑induced bronchoconstriction | 110‑220 | Asthma patients who also suffer nasal symptoms |
| Topical Cream | Skin eczema or atopic dermatitis | 0.05‑0.1% | When skin involvement accompanies respiratory allergies |
For most adults battling seasonal sneezes, the nasal spray is the go‑to option. If you have both asthma and rhinitis, an inhaler can double‑duty, but remember to keep the devices separate to avoid dosing confusion.
Setting Up a Daily Routine
Consistency is the secret sauce. Here’s a practical schedule that slots Fluticasone at the same times each day, paired with complementary treatments.
- Morning (7‑9 AM): If you use a nasal spray, aim for the first dose after brushing your teeth. This timing crowds out morning congestion and helps the medication coat the nasal lining before you head out.
- Mid‑day (12‑1 PM): Take an oral Antihistamine a non‑sedating medication that blocks histamine receptors if you’re active outdoors. The combo of antihistamine + Fluticasone covers both histamine surge and lingering inflammation.
- Evening (6‑8 PM): For inhaler users, administer the dose after dinner. This allows the drug to work overnight, reducing early‑morning wheeze and nasal stuffiness.
- Bedtime (9‑10 PM): Run a quick home‑environment check-close windows, run a HEPA filter, and avoid late‑night pet grooming. A clean room supports Fluticasone’s anti‑inflammatory action.
Tip: Use a pill‑box or smartphone reminder to avoid missed doses. Missing one spray isn’t catastrophic, but irregular use diminishes the drug’s cumulative effect.
Managing Triggers and Complementary Strategies
Fluticasone does a lot, but allergens still love to sneak in. Pair the medication with smart environmental habits.
- Environmental Triggers pollen, dust mites, pet dander, and mold spores: Keep windows shut during high pollen days, wash bedding in hot water weekly, and use allergen‑proof covers.
- Immunotherapy allergy shots or sublingual tablets that gradually desensitize the immune system: Consider it if you need long‑term relief beyond medication.
- Stay hydrated: Warm fluids thin mucus, making it easier for Fluticasone to work.
- Exercise gently: Light cardio boosts airway clearance, but avoid high‑pollen outdoor workouts during peak season.
Monitoring Effectiveness and Side Effects
Track your symptoms for two weeks after starting the regimen. Use a simple chart:
| Day | Runny Nose (0‑5) | Sneezing (0‑5) | Wheeze (0‑5) |
|---|---|---|---|
| 1‑3 | 3 | 4 | 2 |
| 4‑7 | 2 | 3 | 1 |
| 8‑14 | 1 | 1 | 0 |
If scores drop steadily, the dosage is working. Watch for side effects such as nasal dryness, occasional nosebleeds, or a sore throat. Persistent irritation may signal overuse; cut back to the lowest effective dose and discuss alternatives with your clinician.
Common Pitfalls and Pro Tips
- Pitfall: Spraying the nasal spray into the mouth or throat. Pro tip: Aim the nozzle toward the outer wall of the nostril, not the septum.
- Pitfall: Forgetting to clean the inhaler mouthpiece. Pro tip: Rinse with warm water weekly to prevent residue buildup.
- Pitfall: Using the same dose for severe flare‑ups. Pro tip: Talk to your doctor about a short‑term boost rather than self‑escalating.
- Pitfall: Assuming Fluticasone cures allergies. Pro tip: See it as a control tool, not a cure; combine with trigger avoidance and possibly immunotherapy.
Quick Reference Checklist
- Identify your primary formulation (nasal spray, inhaler, or cream).
- Set three fixed daily times for dosing.
- Pair with a non‑sedating antihistamine for extra relief.
- Implement environmental controls (HEPA filter, bedding covers).
- Log symptom scores for two weeks and adjust if needed.
- Watch for dryness, nosebleeds, or throat irritation.
- Schedule a follow‑up with your healthcare provider after 4‑6 weeks.
Frequently Asked Questions
Can I use Fluticasone and a steroid inhaler at the same time?
Yes, if one treats nasal symptoms and the other addresses bronchial asthma. Keep the devices separate and follow dosing instructions for each.
How long does it take for a nasal spray to work?
Most people notice reduced congestion within 12‑24 hours, but full anti‑inflammatory effects can take up to a week of consistent use.
Is it safe to use Fluticasone while pregnant?
Category C data suggest low systemic absorption, but you should discuss any use with your OB‑GYN before starting.
What should I do if I miss a dose?
Take the missed dose as soon as you remember, unless it’s almost time for the next scheduled dose. In that case, skip the missed one and continue with your regular schedule.
Can children use Fluticasone nasal spray?
Yes, formulations for kids as young as 2 years are approved. Doses are lower (typically 50 µg per spray) and should be administered under parental supervision.
By weaving Fluticasone into a predictable daily pattern, backing it up with trigger control, and keeping an eye on how you feel, you’ll turn seasonal sniffles into a manageable nuisance instead of a full‑blown disaster. Give the routine a few weeks, tweak as needed, and enjoy clearer breathing all year round.
fluticasone is the cornerstone of this plan, but success still hinges on consistency and a holistic approach.
Vijaypal Yadav
October 20, 2025 AT 20:55I've been tracking the pharmacokinetics of intranasal corticosteroids for years, so let me break down why the timing in the guide makes sense. The 7‑9 AM window lands right after the circadian rise in nasal vascular permeability, which maximizes mucosal absorption. By pairing the spray with a non‑sedating antihistamine at noon you cover both the early histamine surge and the delayed inflammatory cascade. Evening inhaler dosing capitalizes on the overnight mucociliary clearance slowdown, keeping airway tone stable for the next day. Finally, the bedtime environment check is not just fluff; reducing particulate load prevents rebound irritation that could otherwise blunt the steroid’s effect. Consistency, as the article says, is the real therapeutic driver.
Andrew Hernandez
October 25, 2025 AT 12:01This guide does a solid job laying out a simple schedule. It respects the need for routine without overcomplicating things.
jessie cole
October 26, 2025 AT 18:33Dear colleague, I commend your concise summary and would like to encourage adherence to the proposed timetable. Maintaining a regular dosing schedule has been shown to enhance therapeutic outcomes in clinical trials. Please feel free to reach out if you require further clarification on any of the steps.
Alex Pegg
October 30, 2025 AT 02:08While the article praises Fluticasone’s safety, it glosses over the fact that long‑term steroid exposure can subtly suppress the hypothalamic‑pituitary axis. One should not assume that “minimal systemic absorption” equals zero risk.
JessicaAnn Sutton
November 3, 2025 AT 17:15The exposition adheres to a respectable level of clinical rigor, yet it neglects the ethical dimension of prescribing potent corticosteroids without a comprehensive risk‑benefit discussion. It is incumbent upon healthcare providers to disclose potential mucosal atrophy and the rare possibility of secondary infections. Moreover, the checklist approach, though helpful, may inadvertently promote a checkbox mentality rather than individualized patient care. Ultimately, patient autonomy must remain central to any therapeutic regimen.
barnabas jacob
November 8, 2025 AT 08:21Yo, u gotta peep the pharmaco‑dynamics when u splash that spray. It’s not jus a vibe, it’s a CRF‑mediated downregulation of eosinophil activity. If u skip a dose, the cytokine rebound can cause a flare that’s harder to quash. Also, watch out for nosebleeds – they’re a tell‑tale sign of over‑use, ya?
Ron Lanham
November 22, 2025 AT 05:41Let us consider, for a moment, the broader philosophical implications of regimenting our bodies around a synthetic corticosteroid. The very notion that we must surrender a portion of our autonomy to a manufactured molecule reveals a delicate balance between modern medicine and personal agency. By committing to a fixed schedule, we acknowledge the supremacy of empirical evidence over impulsive desire, yet we also risk reducing our lived experience to a series of timestamps. The author’s recommendation to align nasal spray usage with morning oral hygiene serves as a symbolic gesture, a reminder that even the most mundane rituals can be sanctified by health imperatives. However, this is not merely about convenience; it is about harnessing the body’s own rhythms to maximize drug deposition. In doing so, we exploit the body’s own rhythms, turning a potential weakness into an advantage. The suggested mid‑day antihistamine complement is a strategic maneuver to intercept histamine’s rapid onset, thereby preventing the cascade that would otherwise undermine the steroid’s anti‑inflammatory work. Evening inhaler administration, meanwhile, capitalizes on the nocturnal reduction in sympathetic tone, allowing the medication to linger where it is needed most. One must not overlook the environmental controls outlined in the guide; a clean, filtered living space acts as an unseen co‑therapist, amplifying the pharmacologic effects. The checklist provided is an excellent tool, yet it also risks fostering a mechanistic mindset where patients tick boxes without genuine understanding. This is where education becomes paramount-patients must internalize why each step matters, not merely perform it out of habit. Moreover, while the guide rightly cautions against overuse and the attendant dryness or epistaxis, it should also address the psychological burden of daily medication adherence, which can be a source of anxiety for some individuals. The monitoring chart, though simple, offers a quantitative feedback loop that empowers patients to recognize trends and adjust accordingly. In sum, the integration of Fluticasone into a daily routine, when executed with mindfulness and precision, transcends mere symptom control and becomes an exercise in disciplined self‑care. Let us therefore embrace this regimen not as a chore, but as an affirmation of our commitment to health, rigorously applied and thoughtfully maintained.
Matthew Hall
November 23, 2025 AT 13:13Look, the whole “clean air” narrative is just the tip of a massive cover‑up. Big Pharma and the HVAC industry collude to keep us dependent on aerosolized chemicals, pushing us to spray endlessly while they line their pockets. By following this “routine” you’re basically signing a contract with the establishment that wants you forever inhaling their product.
Deja Scott
November 26, 2025 AT 20:48Consistency truly is the cornerstone of effective allergy management.
Natalie Morgan
December 1, 2025 AT 11:55Great guide it covers timing dosage and environment so readers can take control of their symptoms quickly
Mahesh Upadhyay
December 6, 2025 AT 03:01The plan exemplifies disciplined self‑care; neglecting it is a disservice to one’s own health.