First-Episode Psychosis: Why Early Intervention and Family Support Save Lives

What First-Episode Psychosis Really Means
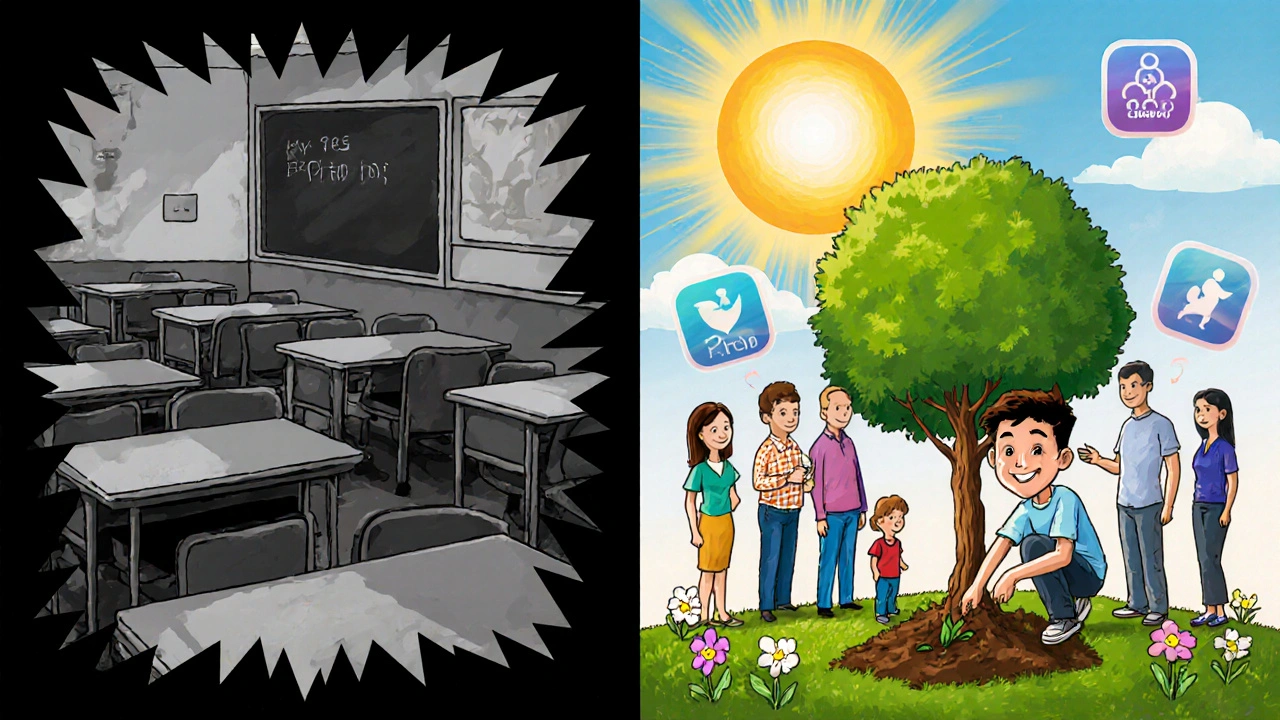
First-episode psychosis (FEP) isn’t just a scary phrase-it’s a real, treatable medical event. It’s when someone experiences psychosis for the first time: hearing voices no one else hears, believing things that aren’t true, speaking in ways that don’t make sense, or acting in ways that seem strange or out of character. These symptoms don’t come out of nowhere. They’re the brain’s way of signaling something is off-often in the teenage or young adult years, between 15 and 35. And here’s the critical part: first-episode psychosis is not a life sentence. It’s a window.
That window is short. The World Health Organization says treatment must start within 12 weeks of the first signs. Why? Because every week without help increases the chance of long-term damage. Studies show that if treatment is delayed by three to six months, people lose ground they may never fully regain-jobs, friendships, school progress, even their sense of self. The brain is still changing during this time. With the right support, it can heal. Without it, it can get stuck in a cycle of worsening symptoms and isolation.
The Science Behind Early Intervention
In 2008, the National Institute of Mental Health launched the RAISE project to test what happens when people with first-episode psychosis get fast, coordinated care. The results were clear: those who got coordinated specialty care (CSC) didn’t just do better-they thrived. Compared to standard treatment, they stayed in therapy longer, improved their quality of life by 25%, reduced symptoms by 32%, and were 40% more likely to return to school or work.
CSC isn’t just one thing. It’s five evidence-based pieces working together. First, case management: someone who helps you navigate doctors, appointments, and benefits-meeting 2-3 times a week when things are rough. Second, medication: not the high doses used for chronic schizophrenia, but lower, smarter doses of second-generation antipsychotics to reduce side effects like weight gain and diabetes. Third, therapy: cognitive behavioral therapy tailored for psychosis, helping people understand their experiences without shame. Fourth, family support: structured sessions that teach loved ones how to respond, reduce stress, and prevent relapse. And fifth, supported employment or education: real help getting back to work or school, not just advice.
The data doesn’t lie. People who start CSC within six months of symptoms have 45% higher chances of symptom remission. Those who stick with it for two years keep their gains. Extend it to four? Sixty-eight percent stay in school or employed. That’s not luck. That’s science.
Why Family Support Isn’t Optional
Families are often the first to notice something’s wrong. But they’re also the most confused. They don’t know if it’s teen rebellion, stress, or something more. They feel helpless. And when they don’t know what to do, they might say the wrong thing-pushing, arguing, or withdrawing-all of which can make symptoms worse.
Family psychoeducation changes that. It’s not a lecture. It’s a structured program-8 to 12 sessions over six months-where families learn what psychosis is, how to recognize early warning signs, how to communicate without triggering stress, and how to support recovery without taking over. Studies show this cuts relapse rates by 25%. That’s not small. That’s life-changing.
One mother in Washington State told her team, “I used to panic when my son talked about the voices. Now I know it’s not about convincing him they’re not real. It’s about asking, ‘How is that making you feel?’” That shift-from fear to curiosity-makes all the difference.
Yet only 55% of families consistently join these programs. Barriers? Shame, lack of time, not knowing where to start. That’s why programs now offer telehealth sessions, evening appointments, and even mobile teams that come to the home. When families are included, recovery isn’t just possible-it’s more likely.

What Coordinated Specialty Care Actually Looks Like
CSC teams aren’t just doctors. They’re a crew: psychiatrists, therapists, case managers, employment coaches, peer support specialists-all working together, meeting weekly to talk about each person’s progress. No one falls through the cracks.
Take the New Journeys program in Washington State. Since 2016, they’ve served over 2,800 young people. Their teams hit a 75%+ fidelity score on quality checks-meaning they’re doing everything right, every time. And the results? The average time between first symptoms and first treatment dropped from 78 weeks to just 26 weeks. That’s a win.
How? They trained 347 clinicians in Massachusetts using 40 hours of classroom learning and 120 hours of supervised practice. They built systems to track every step. They didn’t just hope it would work-they made sure it did.
But here’s the catch: CSC costs more upfront-$8,000 to $12,000 per person per year versus $5,000-$7,000 for standard care. But untreated psychosis? It costs $155 billion a year in the U.S. alone. Lost jobs, emergency rooms, homelessness, incarceration. The math isn’t close. Early intervention saves money, lives, and futures.
The Gaps That Still Exist
Here’s the hard truth: only 18% of people with first-episode psychosis get treatment within the 12-week window. Why? Because in 62% of rural counties, there’s not a single CSC program. Insurance doesn’t always cover it. Only 31 states have Medicaid waivers that pay for all five components. Clinicians burn out. Turnover in CSC teams hits 22% a year. And many doctors still prescribe too-high doses of antipsychotics-despite NICE guidelines saying it’s dangerous and unnecessary.
Some people with severe substance use disorders need dual-diagnosis care first. CSC isn’t magic. It’s not for everyone. But for the vast majority-especially young people without long-term illness-it’s the best shot they’ve got.
Programs like Louisiana’s are finding workarounds: mobile crisis units that show up within 14 days, telehealth for families who can’t drive in, peer mentors who’ve been through it themselves. These aren’t perfect, but they’re progress.
What’s Next? Digital Tools and Bigger Changes
Technology is stepping in. The PRIME Care app, used in 22 CSC programs, lets people log mood, sleep, and symptoms daily. It flags warning signs before a crisis hits. Early results? 30% fewer hospitalizations. That’s huge.
The National Institute of Mental Health is pouring $50 million into research to find biological markers-brain scans, blood tests-that could predict psychosis before it happens. Imagine a teenager with a family history getting a simple test, then getting support before voices start.
But without funding, none of this scales. Dr. Lisa Dixon warns that without stable funding, 80% of young people with FEP won’t get proper care by 2027. Right now, most CSC programs survive on short-term grants. That’s not a system. That’s a patchwork.
The VA/DOD updated their guidelines in September 2023 with 17 new evidence-based rules. SAMHSA gave $25 million in 2023 to expand services. The number of certified CSC programs jumped from 15 in 2010 to 347 in 2023. Progress is real. But it’s not enough.
What You Can Do
If you’re worried about someone you love: don’t wait. Don’t assume it’s just stress. Reach out to a local mental health clinic, a university hospital, or call the National Alliance on Mental Illness (NAMI) helpline. Ask: “Do you have a first-episode psychosis program?” If they say no, ask how to get one started.
If you’re a teacher, coach, or employer: learn the signs. A student who’s suddenly withdrawn, skipping class, talking oddly-this isn’t laziness. It’s a cry for help. Early action saves lives.
If you’re a policymaker: fund CSC. It’s not a luxury. It’s the most cost-effective mental health intervention we have. Every dollar spent now saves $5 in future costs.
This isn’t about fixing broken people. It’s about giving young people back their future. And that’s worth every effort.
Can first-episode psychosis be cured?
Psychosis isn’t something you “cure” like a cold. But with early, coordinated care, most people recover fully-meaning they return to school, work, relationships, and life without ongoing symptoms. The goal isn’t just to stop hallucinations; it’s to rebuild a meaningful life. Many people who get timely treatment never have another episode.
How long does coordinated specialty care last?
Most programs last two years, but research shows extending care to four years keeps people more stable. The first year focuses on crisis and stabilization. The second year builds skills for work, school, and relationships. After that, many transition to ongoing community care-but they don’t disappear. Support continues, just differently.
Are antipsychotic medications dangerous for young people?
They can be, if used wrong. High doses increase risks of weight gain, diabetes, and movement disorders. But CSC uses the lowest effective dose-often half of what’s used for chronic cases. Metabolic health is monitored from day one: weight, waist size, and blood sugar checked every three months. When used correctly, the benefits far outweigh the risks.
What if my family doesn’t believe in mental illness?
Many families struggle with stigma. CSC programs include family education that uses science, not blame. They show brain scans, share research, and explain psychosis as a medical condition-not weakness or bad parenting. One program in Oregon found that after six sessions, 87% of skeptical family members changed their view. Knowledge reduces fear.
Can someone with first-episode psychosis go back to school or work?
Yes-often better than before. Supported employment and education isn’t about forcing someone back too soon. It’s about matching their pace. A coach helps them find a part-time job, adjust their schedule, talk to professors, or request accommodations. In CSC programs, 50-60% get competitive jobs or return to school. In traditional care? Only 20-30%. Recovery isn’t just about feeling better-it’s about doing again.
How do I find a coordinated specialty care program near me?
Start with the Early Psychosis Intervention Network (EPINET) registry online, or call NAMI at 1-800-950-NAMI. Ask your doctor, hospital, or university health center. If none exist locally, ask if they can refer you to a telehealth option. Many programs now offer remote family sessions and virtual therapy. Don’t give up-help is out there, even if it’s not in your town yet.
Final Thought: This Is a Race Against Time
First-episode psychosis isn’t a mystery. We know what works. We’ve tested it. We’ve proven it. The problem isn’t science-it’s access. Too many young people are slipping through the cracks because systems are slow, underfunded, or unaware. But change is possible. It’s already happening-in Washington, in Louisiana, in Massachusetts. It’s happening when families speak up, when schools train staff, when clinics demand funding.
Don’t wait for someone to hit rock bottom. Don’t wait for a crisis. If you see the signs-withdrawal, strange speech, paranoia-act now. Early intervention doesn’t just prevent suffering. It saves potential. And that’s worth fighting for.
Jessica Healey
November 18, 2025 AT 20:51Levi Hobbs
November 20, 2025 AT 15:50henry mariono
November 21, 2025 AT 12:18Sridhar Suvarna
November 22, 2025 AT 05:27Joseph Peel
November 22, 2025 AT 12:10Kelsey Robertson
November 24, 2025 AT 10:16Joseph Townsend
November 24, 2025 AT 16:53Bill Machi
November 25, 2025 AT 09:28Elia DOnald Maluleke
November 26, 2025 AT 05:39satya pradeep
November 27, 2025 AT 14:37Prem Hungry
November 28, 2025 AT 00:08Leslie Douglas-Churchwell
November 29, 2025 AT 00:44shubham seth
November 30, 2025 AT 18:28Kathryn Ware
December 1, 2025 AT 16:18kora ortiz
December 2, 2025 AT 23:55