Effective Antibiotics for Cystitis: Guidance and Best Choices
Cystitis Antibiotic Selector
Select Your Preferred Antibiotic:
Nitrofurantoin
Good for low resistance rates
TMP-SMX
Effective against many pathogens
Fosfomycin
Single-dose option
Fluoroquinolone
Reserved for resistant cases
Select your patient factors and preferred antibiotic, then click "Determine Best Option" to get personalized recommendations.
Key Takeaways
- Most uncomplicated cystitis cases respond to nitrofurantoin, TMP‑SMX, fosfomycin, or a short course of a fluoroquinolone.
- Local resistance patterns dictate the first‑line choice; always ask for a urine culture if symptoms persist.
- Pregnant patients should avoid fluoroquinolones and use nitrofurantoin (except near term) or fosfomycin.
- Kidney function affects drug selection-adjust doses for reduced creatinine clearance.
- Watch for side effects like nausea, photosensitivity, or tendon pain and contact your clinician if they worsen.
cystitis antibiotics are a cornerstone of bladder infection treatment, but picking the right one requires more than a quick Google search. Below you’ll find a practical roadmap that covers what cystitis is, why antibiotics matter, which drugs work best, and how to navigate special situations like pregnancy or kidney disease.
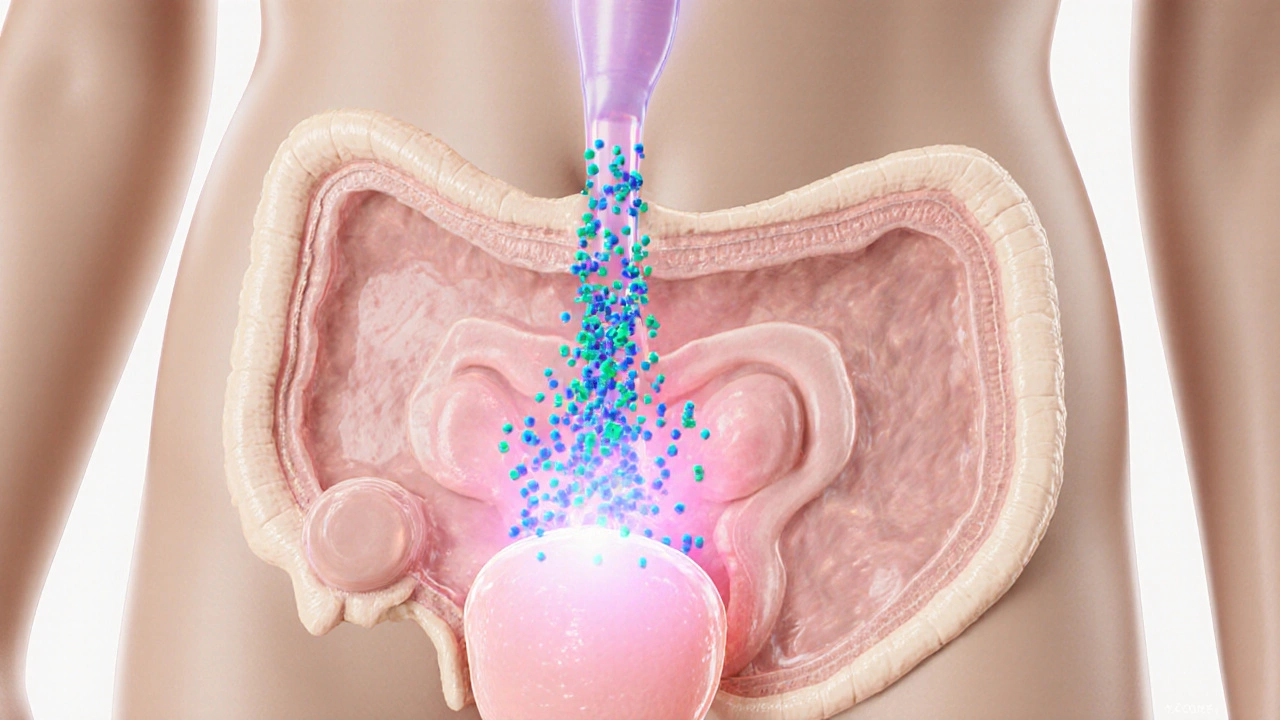
What Is Cystitis?
When doctors talk about cystitis an inflammation of the bladder, usually triggered by bacterial infection, they’re describing a condition that causes burning during urination, frequent urges, and sometimes cloudy urine. In most healthy adults the infection travels up the urethra and colonises the bladder, making it a type of uncomplicated urinary tract infection (UTI).
The most common culprit is Escherichia coli a gram‑negative bacterium responsible for roughly 70‑85% of community‑acquired cystitis cases. Because the bacteria live in the gut, they can hitch a ride to the urinary tract during everyday activities.
Why Antibiotics Are Needed
Symptoms usually resolve on their own within a few days, but without treatment the infection can spread to the kidneys (pyelonephritis) or cause recurrent episodes. Antibiotic therapy lowers bacterial load, shortens symptom duration, and prevents complications. In addition, treating early reduces the risk of developing antibiotic‑resistant strains-an increasingly common public‑health concern.
First‑Line Antibiotics: The Usual Suspects
Guidelines from major health authorities (e.g., IDSA, NICE) recommend a short, oral regimen for uncomplicated cystitis. Below are the four drugs most clinicians prescribe, together with the key facts you’ll need to decide if they’re a good fit.
Nitrofurantoin
Nitrofurantoin a urinary‑concentrating antibiotic that interferes with bacterial DNA synthesis is a favorite because it stays mainly in the bladder, limiting systemic exposure. Typical dose: 100mg twice daily for 5days. It works well when local E.coli resistance is below 10%.
Contraindications include severe renal impairment (creatinine clearance <30mL/min) and late‑term pregnancy (after 36weeks) due to risk of neonatal hemolysis.
Trimethoprim‑Sulfamethoxazole (TMP‑SMX)
Trimethoprim‑sulfamethoxazole a combination that blocks folic‑acid synthesis in bacteria is another first‑line option. Standard regimen: 160mg/800mg (one double‑strength tablet) twice daily for 3days.
Watch out for sulfa allergy, and avoid use in patients with significant liver disease or those taking drugs that can raise potassium levels (e.g., ACE inhibitors).
Fosfomycin
Fosfomycin a single‑dose phosphonic antibiotic that disrupts bacterial cell‑wall synthesis offers convenience: one 3g sachet taken with water, no repeat dosing.
It’s especially handy for patients with adherence concerns, but some regions report rising resistance (up to 15% for E.coli). It’s safe in pregnancy and in patients with modest renal dysfunction.
Ciprofloxacin (Fluoroquinolone)
Ciprofloxacin a broad‑spectrum fluoroquinolone that inhibits bacterial DNA gyrase is reserved for cases where first‑line agents fail or when resistance patterns are unfavorable.
Typical dose: 250mg twice daily for 3days. Side‑effect profile includes tendonitis, QT prolongation, and photosensitivity, so clinicians limit use to short courses and avoid it in pregnant or nursing women.
Choosing the Right Antibiotic: Decision Criteria
Below is a quick checklist you can run through with your clinician or pharmacist:
- Local resistance data: Ask if the clinic tracks antibiograms for E.coli.
- Kidney function: Nitrofurantoin needs adequate glomerular filtration; otherwise consider fosfomycin.
- Allergies: Sulfa allergy rules out TMP‑SMX; fluoroquinolone allergy eliminates ciprofloxacin.
- Pregnancy status: Use nitrofurantoin (except near term) or fosfomycin; avoid fluoroquinolones.
- Adherence potential: Single‑dose fosfomycin works best for busy schedules.
Managing Side Effects and Risks
Even short courses can cause discomfort. Common complaints include:
- Nitrofurantoin - nausea, loss of appetite, occasional lung irritation (rare, usually reversible).
- TMP‑SMX - rash, mild elevations in liver enzymes, rare severe Stevens‑Johnson syndrome.
- Fosfomycin - transient diarrhea, taste alteration.
- Ciprofloxacin - tendon pain, light‑sensitivity, dizziness.
If symptoms worsen after 48hours, stop the medication and contact your provider. They may order a repeat urine culture to verify that the bacteria haven’t developed resistance.
Special Populations
Pregnancy
Bladder infections are common in pregnancy and can jeopardise fetal health if untreated. Nitrofurantoin (first or second trimester) and fosfomycin are considered safe. Fluoroquinolones are contraindicated because they can affect fetal cartilage development.
Kidney Disease
Reduced creatinine clearance hampers drug excretion. Nitrofurantoin is ineffective when clearance <30mL/min, while fosfomycin maintains adequate bladder concentrations. Dose adjustments for TMP‑SMX are needed if eGFR falls below 50mL/min.
Elderly Patients
Age‑related decline in renal function and higher polypharmacy rates raise the chance of drug‑drug interactions. A single dose of fosfomycin often simplifies management and reduces interaction risk.
When to Seek Immediate Care
Most cystitis episodes are manageable at home, but call your doctor or go to urgent care if you notice any of the following:
- Fever over 100.4°F (38°C) or chills.
- Flank pain indicating possible kidney involvement.
- Blood in urine accompanied by severe pain.
- Symptoms persisting beyond 48‑72hours despite appropriate antibiotics.
- New neurological symptoms (e.g., confusion) in older adults.
Comparing Common Antibiotics for Uncomplicated Cystitis
| Antibiotic | Typical Dose & Duration | Contraindications | Resistance Cut‑off (E.coli) |
|---|---|---|---|
| Nitrofurantoin | 100mg PO BID for 5days | CrCl <30mL/min, late‑term pregnancy | <10% |
| TMP‑SMX (160/800mg) | BID for 3days | Sulfa allergy, severe liver disease | ≈15‑20% |
| Fosfomycin | 3g single PO dose | None major; use caution if eGFR <20mL/min | ≈15% |
| Ciprofloxacin | 250mg PO BID for 3days | Pregnancy, tendon disorder, QT‑prolongation | ≈5‑10% |
Putting It All Together: Practical Steps for Patients
- Visit a healthcare professional as soon as symptoms appear.
- Request a urine dipstick or culture-especially if you’ve had recent UTIs.
- Discuss any allergies, current meds, pregnancy status, and kidney function.
- Make sure you understand the prescribed dose and finish the full course.
- Stay hydrated; aim for at least 2L of fluid daily to flush bacteria.
- Track symptoms; if they worsen after 48hours, call back.
Frequently Asked Questions
Can I treat cystitis with over‑the‑counter meds?
Can I treat cystitis with over‑the‑counter meds?
OTC pain relievers like ibuprofen can ease discomfort, but they won’t clear the infection. Antibiotics are required to eradicate the bacteria and prevent complications.
How long does it take for symptoms to improve?
Most patients feel relief within 24‑48hours of starting the correct antibiotic. Complete the prescribed course even if you feel better.
Is it safe to use nitrofurantoin during pregnancy?
Yes, nitrofurantoin is considered safe in the first and second trimesters. Near term (after 36weeks) clinicians often switch to fosfomycin to avoid neonatal hemolysis.
What if I’m allergic to sulfa drugs?
Avoid TMP‑SMX. Nitrofurantoin, fosfomycin, or a short fluoroquinolone course (if no other contraindications) are appropriate alternatives.
Can I take antibiotics for cystitis if I have a urinary catheter?
Catheter‑associated infections often involve different bacteria and may need broader‑spectrum agents like fluoroquinolones or carbapenems. Always have a culture performed.
Deepak Bhatia
October 7, 2025 AT 13:07Looks like you’ve put together a solid guide; I especially like the clear breakdown of each antibiotic and the quick‑check boxes for pregnancy and kidney function. It makes it easy for anyone to pick the right pill without getting lost in medical jargon.
Samantha Gavrin
October 7, 2025 AT 13:40What most people don’t realize is that these “best choice” charts are pushed by big‑pharma lobbyists who want you to stay on cheap, mass‑produced drugs while the newer, safer options get hidden behind paywalls and FDA delays.
NIck Brown
October 7, 2025 AT 14:13Honestly, if you’re still using fluoroquinolones as a first‑line for uncomplicated cystitis you’re ignoring decades of resistance data-stick to nitrofurantoin or fosfomycin unless culture proves otherwise.
Andy McCullough
October 7, 2025 AT 15:03When selecting an antimicrobial for cystitis, the pharmacokinetic profile is paramount because drug concentration in the urine directly correlates with bactericidal activity. Nitrofurantoin, for instance, achieves high urinary excretion (>80% of the administered dose) while maintaining low systemic exposure, which reduces off‑target toxicity. However, its efficacy drops sharply when creatinine clearance falls below 60 mL/min, necessitating dose adjustment or an alternative agent. TMP‑SMX offers broad coverage against E. coli and other Enterobacteriaceae, but the prevalence of sulfonamide resistance in the community has risen to roughly 20‑30% in many regions, making local antibiograms essential before prescribing. Fosfomycin, administered as a single 3 g dose, provides a convenient option for patients with adherence challenges, yet its penetration into the bladder wall is modest, so it is best reserved for uncomplicated cases without recent antimicrobial exposure. Fluoroquinolones possess excellent tissue penetration and a low resistance threshold, which is why guidelines reserve them for cases where first‑line agents are contraindicated or have failed. In pregnant patients, nitrofurantoin is generally safe except during the third trimester due to the risk of neonatal hemolysis, while TMP‑SMX should be avoided near term because of potential kernicterus. Fosfomycin remains a viable alternative throughout pregnancy, provided renal function is adequate. Renal impairment also impacts drug clearance; for example, reduced glomerular filtration prolongs the half‑life of nitrofurantoin, increasing the risk of pulmonary toxicity with prolonged courses. Dose modification algorithms recommend 100 mg twice daily for patients with eGFR 30‑60 mL/min, or switching to a non‑renal‑cleared agent such as cefpodoxime if eGFR falls below 30. Local resistance patterns should drive empirical therapy: in regions where E. coli resistance to nitrofurantoin exceeds 10%, TMP‑SMX or fosfomycin become more attractive first‑line choices. Moreover, culture and sensitivity testing is indispensable when symptoms persist beyond 48‑72 hours despite appropriate therapy, as this may indicate resistant organisms or atypical pathogens like Klebsiella or Proteus. Side‑effect profiles also influence decision‑making; patients reporting photosensitivity should avoid fluoroquinolones, whereas those with a history of tendon disorders should steer clear of this class altogether. Finally, patient education on proper drug intake-taking nitrofurantoin with food to enhance absorption, or spacing TMP‑SMX doses to minimize gastrointestinal upset-can improve compliance and outcomes. By integrating pharmacodynamics, renal function, pregnancy status, and local resistance data, clinicians can tailor therapy to achieve rapid symptom resolution while mitigating the development of resistance.
Zackery Brinkley
October 7, 2025 AT 15:37Great job laying out the steps; remembering to check kidney function first can save a lot of headaches later on.
Luke Dillon
October 7, 2025 AT 16:10It’s tough when you feel the system is pushing certain meds, but the safety data for the listed drugs is still solid for most people. Just keep an eye on how you feel and talk to your doctor if anything seems off.
Elle Batchelor Peapell
October 7, 2025 AT 17:00Isn’t it funny how a tiny bladder infection can spark a whole cascade of choices, each with its own ethical and practical footprint?
Jeremy Wessel
October 7, 2025 AT 17:33Pick the drug that matches your health status and local resistance data.
Laura Barney
October 7, 2025 AT 18:07Imagine the bacteria as tiny invaders; nitrofurantoin is the swift arrow that homes in on them, while fosfomycin is the sudden flashbang that knocks them out in one burst-both can be heroic, but only if the battlefield (your urinary tract) is ready for them.
Jessica H.
October 7, 2025 AT 18:57While the guide offers a useful overview, it neglects to address the emerging carbapenem‑resistant Enterobacteriaceae strains that, albeit rare, are increasingly implicated in recurrent cystitis cases, thereby limiting its applicability for patients with a history of multidrug‑resistant infections.
Tom Saa
October 7, 2025 AT 19:30One could argue that the very act of categorizing infections into “simple” and “complex” reflects our desire to impose order on a fundamentally chaotic biological reality.
John Magnus
October 7, 2025 AT 20:20Stop treating cystitis as a “one‑size‑fits‑all” scenario; you need to run a susceptibility panel before you slap on a generic five‑day course, especially in regions where ESBL‑producing E. coli prevalence exceeds 15 % and empiric nitrofurantoin failure rates are climbing.
Marc Clarke
October 7, 2025 AT 20:53Honestly, if you’re just dealing with a first‑time UTI, start with nitrofurantoin, watch the symptoms, and only jump to the more intense antibiotics if you don’t improve in a couple of days. It’s a low‑risk, high‑reward move for most people.